5 Minutes
Alzheimer’s Disease: A Global Health Challenge
Alzheimer’s disease is the most prevalent form of dementia worldwide, representing 60% to 70% of all dementia diagnoses. With a new case developing roughly every three seconds globally, the disease poses urgent medical and social challenges. Despite decades of neuroscience breakthroughs, an effective cure remains elusive, primarily because Alzheimer’s disease is a complex disorder with several contributing factors—many of which are not yet fully understood.
The Science Behind Alzheimer’s: Proteins at the Core
Central to Alzheimer’s pathology are two abnormal proteins: amyloid-beta and tau. Research has shown that amyloid-beta forms sticky plaques on the outer surfaces of neurons, interfering with their ability to communicate. Inside nerve cells, tau protein accumulates and becomes twisted into so-called “neurofibrillary tangles,” disrupting normal cellular function and leading eventually to cell death. These plaques and tangles are the defining features of Alzheimer’s brains and have been the focal point of most scientific inquiry for decades.
This well-established concept—often called the amyloid hypothesis—has shaped the majority of modern Alzheimer’s research and given rise to new treatments. Monoclonal antibody drugs designed to clear amyloid-beta from the brain have recently gained regulatory approval. However, such therapies are only effective in the early stages of Alzheimer’s and come with significant limitations, including serious side effects such as brain swelling and bleeding. Notably, these drugs focus solely on amyloid-beta, leaving tau pathology unmitigated.
Helicobacter pylori: From Stomach Ulcers to Brain Health?
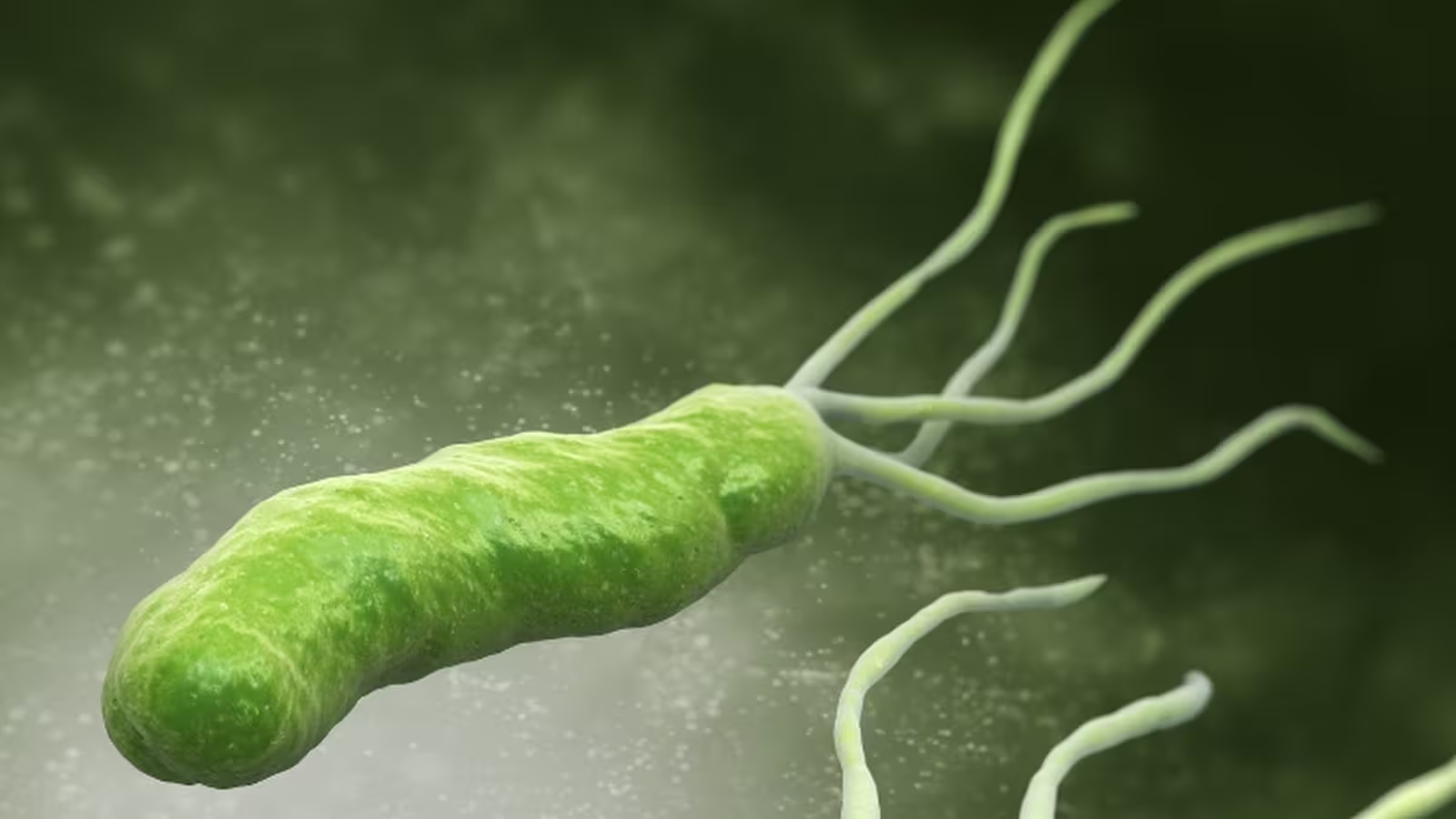
In an unexpected scientific breakthrough, recent studies have identified a molecule from Helicobacter pylori—a bacterium best known for causing stomach ulcers—that can inhibit the accumulation of both amyloid-beta and tau proteins. This discovery suggests the surprising possibility that a microbe once considered purely harmful may hold crucial clues for neurodegenerative disease prevention.
The research began with an exploration of microbial communities called biofilms. Some bacteria, including H. pylori, exist in protective biofilms that are reinforced by protein aggregates resembling the amyloids found in the human brain. Scientists wondered if H. pylori could impact human amyloid formation through similar mechanisms.
The CagA Protein: A Double-Edged Sword
Focus shifted to CagA, a protein produced by H. pylori. All CagA proteins have two regions: the C-terminal segment known for its damaging effects in human cells, and the N-terminal region, which remained poorly characterized. When researchers isolated the N-terminal fragment, named CagAN, they found it significantly reduced amyloid formation in Escherichia coli and Pseudomonas bacteria. Encouraged by these findings, the team tested whether CagAN could also affect human amyloid-beta.
Disrupting Toxic Protein Buildup in the Lab
In controlled laboratory experiments, amyloid-beta molecules were incubated—some exposed to CagAN and others as untreated controls. Using advanced techniques such as fluorescence readings and electron microscopy, the researchers observed a dramatic reduction in amyloid aggregation among the treated samples. Even at very low concentrations, CagAN almost completely prevented the formation of amyloid-beta clusters.
To uncover the underlying mechanisms, the scientists employed nuclear magnetic resonance (NMR) spectroscopy and computer-based molecular modeling. Their analyses revealed that CagAN interacts directly with amyloid-beta to block its aggregation. Surprisingly, CagAN also inhibited the clumping of tau proteins, suggesting a multi-targeted mode of action.

Implications: A Broader Therapeutic Potential
Further experiments extended the promise of this discovery beyond Alzheimer’s. The same bacterial protein fragment effectively stopped the aggregation of islet amyloid polypeptide (IAPP)—linked to type 2 diabetes—and alpha-synuclein, a protein thought to drive Parkinson’s disease. Since these disorders all involve the harmful build-up of amyloid aggregates, CagAN might disrupt a shared pathological process across multiple diseases.
What Do These Findings Mean for Future Alzheimer’s Treatments?
The revelation that a Helicobacter pylori protein fragment can block two of Alzheimer’s most notorious protein culprits has major implications. In the future, bacterial proteins such as CagAN—or drugs inspired by them—could be designed to intercept the earliest stages of neurodegenerative diseases, potentially before irreversible brain damage occurs.
These laboratory results suggest that some bacteria traditionally blamed for disease may also harbor molecules capable of fostering health. Rather than striving to eliminate all microbes indiscriminately, precision medicine may need to better differentiate between harmful and potentially beneficial microbial factors.
Caveats and Next Steps
It’s important to note that this research is still at an early, experimental stage. All current findings come from laboratory (in vitro) experiments, with studies in animal models and eventually humans yet to come. The scientists are now focused on unraveling exactly how CagAN disrupts amyloid formation at a molecular level, and testing its efficacy and safety in living systems.
Additionally, previous research into links between H. pylori infection and Alzheimer’s disease has yielded mixed results. This new evidence adds nuance to the discussion, suggesting that while certain H. pylori components can be harmful, others may offer protective effects—possibly depending on strain, context, or even individual patient biology.
Conclusion
Recent discoveries in Alzheimer’s disease research underscore the intricate relationship between the microbiome and brain health. The identification of a Helicobacter pylori protein capable of blocking both amyloid-beta and tau aggregation opens new avenues for drug development in the fight against Alzheimer’s, and potentially other amyloid-related disorders like type 2 diabetes and Parkinson’s disease. These insights challenge the traditional narrative that all bacteria are deleterious, pointing towards a future in which therapies may leverage beneficial microbial molecules. As science advances, more precise and personalized strategies will likely become central to the management and prevention of complex neurodegenerative diseases.
Source: theconversation


Comments