5 Minutes
The Stealthy Threat of Pancreatic Cancer
The pancreas is an often-overlooked organ, yet it plays a critical role in human health by orchestrating digestion and regulating metabolism through the secretion of enzymes and hormones. When this vital system malfunctions, the impact can be life-altering. Pancreatic cancer, particularly pancreatic ductal adenocarcinoma (PDAC), is deemed one of the deadliest forms of cancer due to its low survival rates and tendency to remain asymptomatic until reaching advanced, less treatable stages. According to recent statistics from the United Kingdom, between 2017 and 2019, over 10,700 individuals were diagnosed and 9,500 lost their lives to pancreatic cancer, highlighting its alarming lethality and increasing prevalence.
PDAC forms in the pancreatic duct, the conduit that connects the pancreas to the small intestine. Tumors growing in this area may obstruct digestive enzyme flow, disrupt energy metabolism, and exacerbate chronic fatigue—symptoms so mild and nonspecific that they often go unnoticed. This insidious progression is partly why PDAC is often called the "silent killer."
Turning to the Microbiome: Stool Testing as a Diagnostic Frontier
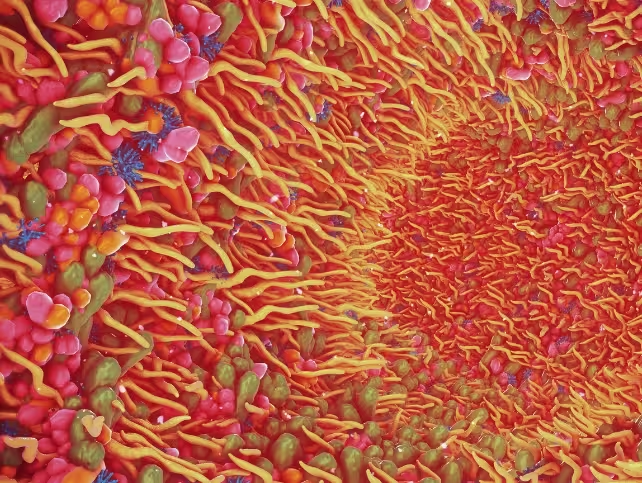
In pursuit of earlier and more accurate detection of pancreatic cancer, researchers are now focusing on an unusual but accessible resource: stool samples. While the idea of diagnosing cancer from fecal matter may seem unconventional, accumulating evidence suggests that our waste holds a wealth of health data. Central to this new diagnostic approach is the human gut microbiome—a complex ecosystem comprised of trillions of bacterial cells that actually outnumber human cells in the body. These microbial inhabitants not only aid digestion and immune function but also provide a dynamic snapshot of our physiological state, including disease onset and progression.
Because PDAC often arises in the portion of the pancreas that empties into the gut, analyzing stool samples offers a non-invasive and practical means to gauge internal health. This emerging method capitalizes on the fact that changes in gut bacteria can reflect the early stages of cancer, sometimes before clinical symptoms develop.
International Research Validates Gut Microbiome-Based Screening
Global scientific collaborations are accelerating the development of microbiome-based diagnostics. Landmark studies from Japan, China, and Spain have validated the link between gut bacteria profiles and pancreatic cancer, with the most recent breakthrough emerging from a 2025 joint effort by researchers in Finland and Iran. In this study, scientists collected stool samples from diverse populations, extracting bacterial DNA and employing 16S rRNA gene amplicon sequencing—a method that sequences a specific gene found in all bacteria to both classify and quantify species present.
The findings were compelling: individuals with PDAC exhibited noticeably reduced gut bacterial diversity, with some species overrepresented and others depleted compared to healthy controls. Notably, the research team developed an artificial intelligence (AI) model capable of distinguishing between cancer patients and healthy individuals solely based on their gut microbiome profiles, demonstrating the potential for accurate, minimally invasive screening.
Technological Advances in Microbiome Research
While 16S rRNA sequencing provides valuable insight, cutting-edge methods such as shotgun metagenomic sequencing are now enabling scientists to capture the entire genetic repertoire of bacteria present in stool samples, offering even higher detection accuracy and revealing microbiome dynamics in greater detail. This technology can even track recent bacterial transmission between individuals, pushing the boundaries of infectious disease research and personalized medicine.
Such advances are prompting a paradigm shift: rather than seeing health solely as a function of human genetics, there is growing recognition that the human body and its resident microbiota form interdependent ecological networks—“the human-plus-microbiome” perspective. These discoveries are rapidly transforming how diseases like cancer are understood, diagnosed, and, potentially, prevented.
Implications Beyond Pancreatic Cancer
The diagnostic promise of microbiome analysis extends well beyond pancreatic malignancies. At the Quadram Institute, researchers are applying similar sequencing and computational approaches to colorectal cancer research, having already processed thousands of stool samples to reconstruct bacterial genomes and elucidate their interactions with the human host in the context of cancer.
Emerging evidence suggests a bidirectional relationship between cancer and the gut microbiome: specific bacterial patterns can herald disease, and conversely, cancer can reshape the microbiome itself—a phenomenon also observed in other disorders such as Parkinson's disease. As Professor Tim Spector, a leading microbiome researcher, remarks, “Understanding the interplay between our microbes and diseases opens up a new universe for early diagnostics and innovative therapies.”
Biotechnological advancements and breakthroughs in artificial intelligence are making it increasingly feasible to unravel these complex interactions. AI-driven models can swiftly process vast amounts of genetic and clinical data, uncovering patterns and markers that would be impossible to detect through traditional analysis.
Future Prospects and Clinical Translation
Although microbiome-based cancer diagnostics remain an evolving field, these discoveries offer hope for earlier intervention, improved patient outcomes, and less invasive screening protocols. Bringing such tools into routine clinical practice entails rigorous validation, long-term studies, and careful consideration of population diversity and disease variability.
The integration of microbiome analysis into cancer care workflows could revolutionize preventative medicine, allowing for earlier detection of diseases that currently evade prompt diagnosis. As researchers continue to map the “microbial fingerprint” of various cancers and chronic conditions, the potential to develop personalized risk assessments and targeted therapeutic strategies grows ever stronger.
Conclusion
Efforts to decode the gut microbiome are reshaping our understanding of health and disease by revealing hidden biological signals in the substances we routinely discard. The prospect of using stool analysis to detect pancreatic cancer marks a transformative step—one that could save thousands of lives by catching the silent killer at its earliest, most treatable stage. Continued innovation in genomics, biotechnology, and artificial intelligence is crucial for unlocking the promise of microbiome-based diagnostics, bringing us closer to a future where early, precise, and non-invasive cancer screening is the standard of care.
Source: theconversation



Comments