4 Minutes
Understanding the Viral Impact on Psychiatric Disorders
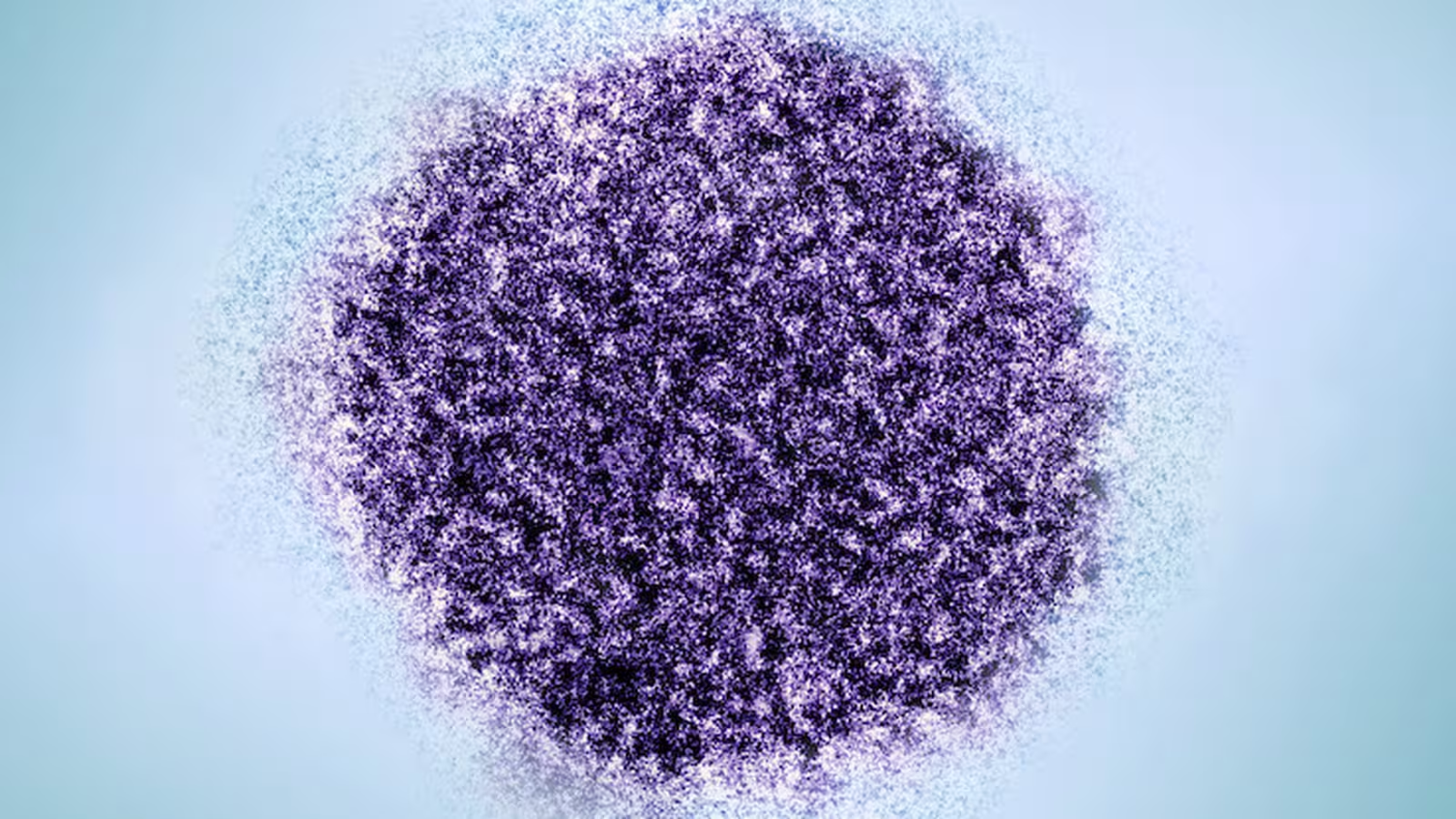
Groundbreaking new research has revealed traces of the hepatitis C virus (HCV) and other viral species in the brain lining—the choroid plexus—of individuals diagnosed with schizophrenia and bipolar disorder. This discovery, led by scientists at Johns Hopkins University, deepens our understanding of the connection between infectious diseases and severe mental health conditions, highlighting possible avenues for novel treatments.
Scientific Context: Exploring the Brain's Protective Lining
Over the years, epidemiological studies have suggested correlations between certain viral infections and major psychiatric disorders, including schizophrenia, bipolar disorder, and major depression. However, direct detection of viral material inside human brain tissue has been exceptionally rare.
Seeking answers, researchers focused on the choroid plexus—a specialized structure made up of capillaries and connective tissue. This region generates cerebrospinal fluid, serving as a protective cushion for the brain and spinal cord, facilitating nutrient exchange, and removing metabolic waste. The choroid plexus is also recognized as a frequent viral target due to its unique location and role as a barrier between blood and brain tissue.
Major Findings: A Closer Examination of Brain Tissue
The research team analyzed postmortem brain samples from individuals with schizophrenia, bipolar disorder, major depression, and matched control subjects. These samples were sourced from the Stanley Medical Research Institute, a premier resource for the study of neuropsychiatric diseases.
To detect hidden viral sequences, scientists employed the Twist Comprehensive Viral Research Panel, a next-generation sequencing tool capable of identifying over 3,000 viral species. The results were striking: 13 different viruses were found in the choroid plexus of study subjects, with the hepatitis C virus exhibiting an especially strong association with both schizophrenia and bipolar disorder compared to healthy controls.
While multiple viruses appeared more frequently in affected individuals, statistical analysis revealed that only HCV showed a significant connection to these psychiatric disorders. This prompted further investigation into potential mechanisms linking HCV infection to mental health symptoms.
Expanding the Search: Large-Scale Health Data Analysis
In the study's second phase, the team broadened their analysis using the TriNetX global health records database, comprising data from over 285 million patients. This large-scale epidemiological inquiry confirmed that hepatitis C infection was more common among individuals with schizophrenia (3.5%) and bipolar disorder (3.9%) compared to those with major depression (1.8%) or the general population (0.5%).
These findings underscore a robust relationship between HCV and serious psychiatric disorders that goes beyond chance, suggesting further research is necessary to unravel cause and effect and explore potential implications for patient care.
Insights from the Hippocampus
To determine whether viral particles had infiltrated deeper brain regions, the researchers also examined the hippocampus—a critical area involved in memory and emotional regulation. No viral traces were detected in the hippocampus itself, implying the brain’s protective barriers were effective at containing pathogens. However, individuals with HCV in the choroid plexus exhibited altered gene expression in the hippocampus, indicating that viral presence in the brain’s lining may still influence neurological function indirectly.
Implications for Future Research and Treatment
While these findings do not suggest that all individuals with schizophrenia or bipolar disorder harbor hepatitis C or other viruses, they point to a potentially treatable biological factor within a subset of patients. As Dr. Sarven Sabunciyan, lead neuroscientist on the study, explains:
“Our findings show that it’s possible some people may be experiencing psychiatric symptoms due to an underlying infection. Since hepatitis C is a treatable condition, antiviral drugs could offer new hope for select patients struggling with mental health symptoms.”
Further research is urgently needed to clarify the biological mechanisms that allow viruses to affect the brain from its outer layers, and to determine if antiviral therapies could mitigate psychiatric symptoms in affected individuals.
Conclusion
This pioneering study provides fresh evidence linking hepatitis C virus infection to severe psychiatric disorders, notably schizophrenia and bipolar disorder, by identifying viral material in the brain’s protective lining. The findings invite a reevaluation of how infections might influence brain health and pave the way for innovative therapies targeting the root causes of psychiatric illness. Continued exploration in this field could lead to transformative new strategies for understanding and treating mental health disorders worldwide.
Source: nature


Comments