4 Minutes
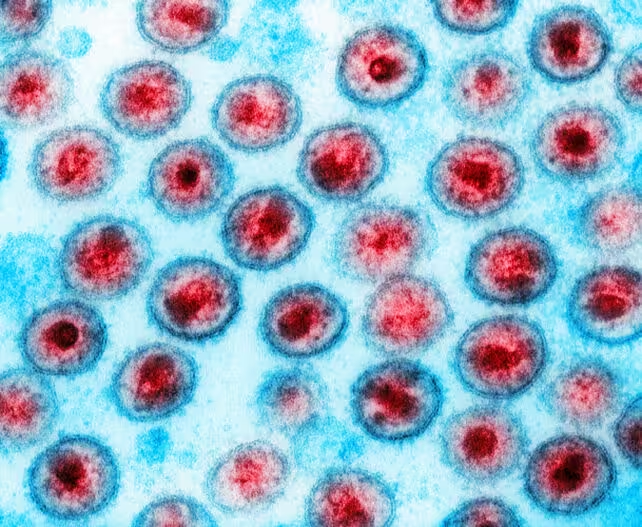
FDA Approves Landmark HIV Prevention Injection
In a milestone for infectious disease prevention, the United States Food and Drug Administration (FDA) has approved a new long-acting HIV prevention medication, marking a significant advance in global public health efforts. The newly authorized drug, lenacapavir, branded as Yeztugo, is the first injectable pre-exposure prophylaxis (PrEP) administered just twice a year to protect against HIV infection—a major development for the prevention of the virus that causes AIDS.
Scientific Background: From Daily Pills to Long-Acting PrEP
Pre-exposure prophylaxis (PrEP) has revolutionized HIV prevention over the past decade, but existing options have faced barriers to widespread adoption. Traditional PrEP regimens, such as the well-known oral medication Truvada, require strict daily adherence to maintain protection, limiting their effectiveness on a global scale. The new landscape-changing approval of lenacapavir offers an alternative—a biannual injection that could vastly improve access and adherence, especially in populations at high risk for HIV exposure.
Daniel O'Day, Chairman and CEO of Gilead Sciences, noted, "This is a historic day in our decades-long battle against HIV."
Clinical Trial Results Demonstrate Exceptional Efficacy
Rigorous clinical trials underpin Yeztugo’s FDA approval. In one pivotal study across sub-Saharan Africa, more than 2,000 women participated. Not a single HIV infection occurred among those receiving lenacapavir, demonstrating a 100% reduction in risk and outperforming daily oral PrEP.
A parallel trial involved over 2,000 men and gender-diverse individuals at elevated risk for HIV. Only two infections were recorded, translating to a prevention rate exceeding 99.9%, again surpassing conventional treatments like Truvada.
The most commonly reported side effects included mild injection site reactions, headache, and occasional nausea, all largely manageable. These groundbreaking trial results were published in The New England Journal of Medicine, and lenacapavir was subsequently named "Breakthrough of the Year" by Science magazine for 2024.
Global Implications and Challenges: Access and Pricing
Despite the promise of a highly effective, twice-yearly HIV prevention tool, the global impact will depend heavily on pricing and accessibility. Existing long-acting alternatives such as cabotegravir, approved in 2021 and requiring injection every two months, are priced in the tens of thousands of dollars per year, hampering their widespread adoption.
Price projections for Yeztugo remain uncertain, with analysts anticipating an initial annual US market price around $25,000. Lenacapavir’s previous list price as an HIV treatment stands at $39,000 per year, though preventive pricing may be considerably lower. The steep cost has led public health advocates and scientists, including Andrew Hill of Liverpool University, to call for dramatic reductions. Hill’s research team demonstrated that lenacapavir could be mass-produced for as little as $25 per person annually.
Winnie Byanyima, United Nations Under-Secretary-General, commented, "Lenacapavir could be the tool we need to control new infections—provided it is affordable and accessible to all who could benefit."
To foster global access, Gilead has signed agreements with six pharmaceutical manufacturers to produce generic versions for up to 120 low- and middle-income countries. However, large-scale availability is still months or years away due to regulatory processes, manufacturing setup, and logistical hurdles.
Collaborative Efforts and the Future of HIV Prevention
Complementing efforts to expand access, Gilead struck a deal in partnership with the Global Fund—an international financing organization co-founded by the United Nations and the US President's Emergency Plan for AIDS Relief (PEPFAR)—to supply millions of doses for vulnerable populations.
However, recent funding cuts to vital US programs such as PEPFAR have introduced uncertainty, potentially delaying or limiting distribution in regions most urgently needing effective HIV prevention.
Lenacapavir’s approval is expected to catalyze further research into long-acting antiretroviral drugs and potentially pave the way for similar advances in infectious disease prevention worldwide.
Conclusion
The FDA’s approval of lenacapavir marks a transformative step forward in the science of HIV prevention. With twice-yearly injections offering more than 99.9% protection, the technology promises to reshape how at-risk populations can safeguard their health and reduce new HIV infections globally. Yet, realizing the full benefit of this breakthrough will depend on delivering the drug at an accessible price and ensuring widespread availability—making it a true tool for ending the HIV pandemic.
Source: sciencealert


Comments