4 Minutes
Rethinking OCD: From Brain Disorder to Gut Connection
Obsessive-compulsive disorder (OCD) has long been considered one of the most difficult mental health conditions to treat, affecting up to 3 percent of the global population. Traditionally, the origins of OCD have been attributed primarily to brain chemistry, genetic predisposition, and environmental factors. However, groundbreaking new research is challenging this perspective, pointing instead to the gut microbiome—the diverse ecosystem of bacteria residing in our digestive tracts—as a potentially key contributor to the development and progression of OCD.
Scientific Background: The Gut-Brain Axis and Mental Health
The concept of the "gut-brain axis" has gained increasing attention in the scientific community. This term describes the complex bidirectional communication network linking the gastrointestinal tract and the central nervous system. Emerging evidence indicates that intestinal microbiota can influence mental health, impacting conditions such as depression, anxiety, and neurodevelopmental disorders. Until now, studies had hinted at possible correlations between gut bacterial composition and OCD. Yet, definitive evidence linking causation rather than mere association has been elusive.
Key Research Insights: Genetic Evidence Links Gut Bacteria to OCD Development
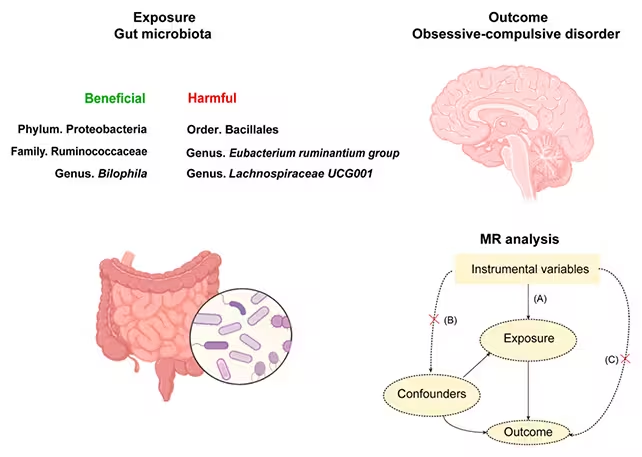
A recent study led by scientists at Chongqing Medical University in China provides the most compelling argument to date for a causal relationship between gut microbiota and OCD risk. To move beyond correlations, the research team applied Mendelian randomization—a genetic epidemiology technique that leverages inherited genetic variations to infer cause-and-effect relationships.
The scientists analyzed two extensive datasets: one included genetic and microbial data from more than 18,000 individuals, while another comprised genetic data from nearly 200,000 individuals diagnosed with OCD. By comparing these datasets, they identified specific bacterial families whose presence or absence appeared directly associated with the disorder.
Their findings revealed that three types of gut bacteria—Proteobacteria, Ruminococcaceae, and Bilophila—might offer a protective effect against OCD. Conversely, higher abundance of Bacillales, Eubacterium, and Lachnospiraceae UCG001 was linked to an increased risk of developing OCD. Notably, several of these bacteria have also been associated with other mental health conditions; for instance, reduced levels of Ruminococcaceae have previously been observed in individuals with depression.
Implications for OCD Treatment and Prevention
This research points toward new pathways for both understanding and addressing obsessive-compulsive disorder. Currently, standard treatments—such as cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs)—are effective for many, but 25–40 percent of patients experience inadequate relief or none at all. Targeting the gut microbiome could provide an entirely new therapeutic angle, potentially improving outcomes for those who do not respond to conventional interventions.
However, the study authors emphasize that more investigation is required before clinical applications can be developed. Larger, longitudinal studies involving more diverse populations, as well as in-depth analysis of bacterial species and their metabolic byproducts, will be crucial to validate these findings and further unravel the role of the gut-brain axis in OCD.
Quotes From Leading Researchers
"Previous studies have indicated a potential link between the gut microbiota and OCD. However, the exact causal relationship remains uncertain," the research team writes. They add, "Our analysis suggested that specific gut microbiota might have a causal relationship with OCD, revealing potential intervention strategies for the prevention and treatment of this disorder."
Conclusion
This milestone study marks a significant advance in our understanding of the biological underpinnings of obsessive-compulsive disorder. By establishing a probable direct link between gut bacteria and OCD, the findings not only deepen scientific knowledge of the gut-brain axis but also signal new directions for prevention and treatment. While practical therapies based on reshaping the gut microbiome may still be years away, these discoveries offer renewed hope for millions of people affected by OCD—and for the clinicians and families supporting them.



Comments