5 Minutes
Background: why this matters for type 1 diabetes
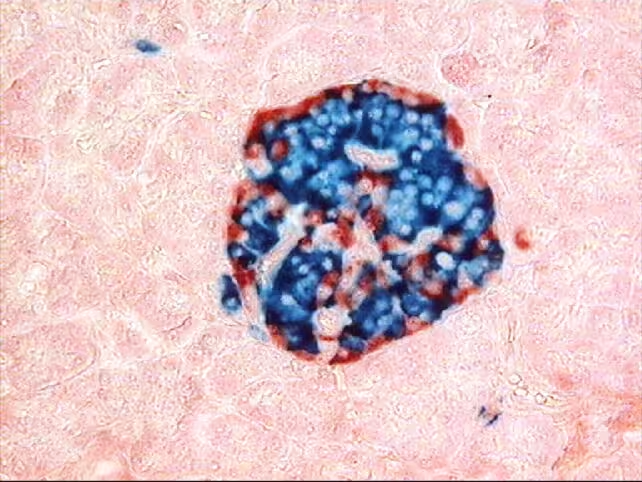
Type 1 diabetes is an autoimmune condition in which the body's immune system destroys pancreatic islet cells that produce insulin. Standard treatment requires lifelong insulin injections and careful glucose management. Replacing damaged islet cells with functional donor cells — an approach known as islet transplantation — has long been explored as a route to restore physiological insulin secretion. However, transplanted cells are typically recognized as foreign by the recipient's immune system, necessitating immunosuppressant drugs that carry serious infection and malignancy risks.
Proof-of-concept human transplant using gene-edited islets
In a landmark proof-of-concept study, a 42-year-old man who has lived with type 1 diabetes since age five received donor pancreatic islet cells that were genetically edited to evade immune detection. The cells were delivered via multiple injections into muscle tissue in the forearm. Over the subsequent 12 weeks the grafted islets began producing insulin in response to rises in blood glucose — for example after meals — and, crucially, the patient did not require systemic immunosuppressive therapy.
Genetic editing strategy
Researchers used CRISPR gene-editing to introduce three modifications to the donor islet cells before transplantation. Two edits reduced the expression of specific antigens used by adaptive T cells to identify and attack non-self tissue, while the third increased production of CD47, a cell-surface protein that inhibits innate immune responses. The triple-edit approach was designed to blunt both adaptive (T cell) and innate (natural killer cells and macrophages) arms of the immune system without suppressing the recipient's overall immunity.
Not all cells in the graft carried successful edits. That variation provided an internal control: unedited cells were rapidly eliminated by T cells, cells with only the antigen-reduction edits were still attacked by natural killer cells and macrophages, and only cells that carried all three successful edits survived long enough to remain functional. The presence of sufficient triple-edited islets in the graft maintained insulin production during the observation window.
Key results and implications
This is the first reported human case in which genetically edited islet cells functioned in a recipient without the use of immunosuppressants. Preclinical studies in nonhuman primates and rodents had suggested the approach could work, but previous human islet transplants that succeeded typically required immunosuppression. Avoiding lifelong immunosuppressive drugs would dramatically reduce the long-term health risks for transplant recipients and broaden the clinical applicability of cell therapies.
Beyond diabetes, the technique suggests a generalizable platform for making other donor cell and tissue grafts less visible to the host immune system. If reproducible and safe in larger trials, CRISPR-enabled immune-evasive engineering could reduce or eliminate the need for immunosuppression in a range of allogeneic transplants.
Related developments and context
Parallel advances include autologous approaches that avoid immune mismatch altogether: for example, a recent case in China reported a young woman who received insulin-producing cells derived from her own stem cells and achieved sustained glucose control without donor-derived immune barriers. Both autologous cell therapies and immune-evasive allogeneic grafts are active research directions, each with distinct advantages and technical challenges.
Expert Insight
"This outcome is a pivotal proof of concept," says Dr. Elena Martín, a fictional immunologist familiar with transplant immunology. "The combination of antigen downregulation and CD47 upregulation addresses both adaptive and innate immunity — that's the key innovation. But we need larger, controlled trials to confirm durability, rule out off-target effects of editing, and verify long-term safety." Experts emphasize careful monitoring for potential unintended consequences, such as altered graft behavior or rare immune complications.
Conclusion
The reported case represents a major step toward cell-based cures for type 1 diabetes by demonstrating that CRISPR-edited islet cells can function in a human host without systemic immunosuppression. While preliminary, the result opens new paths for safer, more broadly applicable cell therapies and highlights the need for continued clinical trials to assess efficacy, safety, and long-term outcomes.
Source: nejm


Leave a Comment