4 Minutes
menstrual blood as an overlooked diagnostic resource
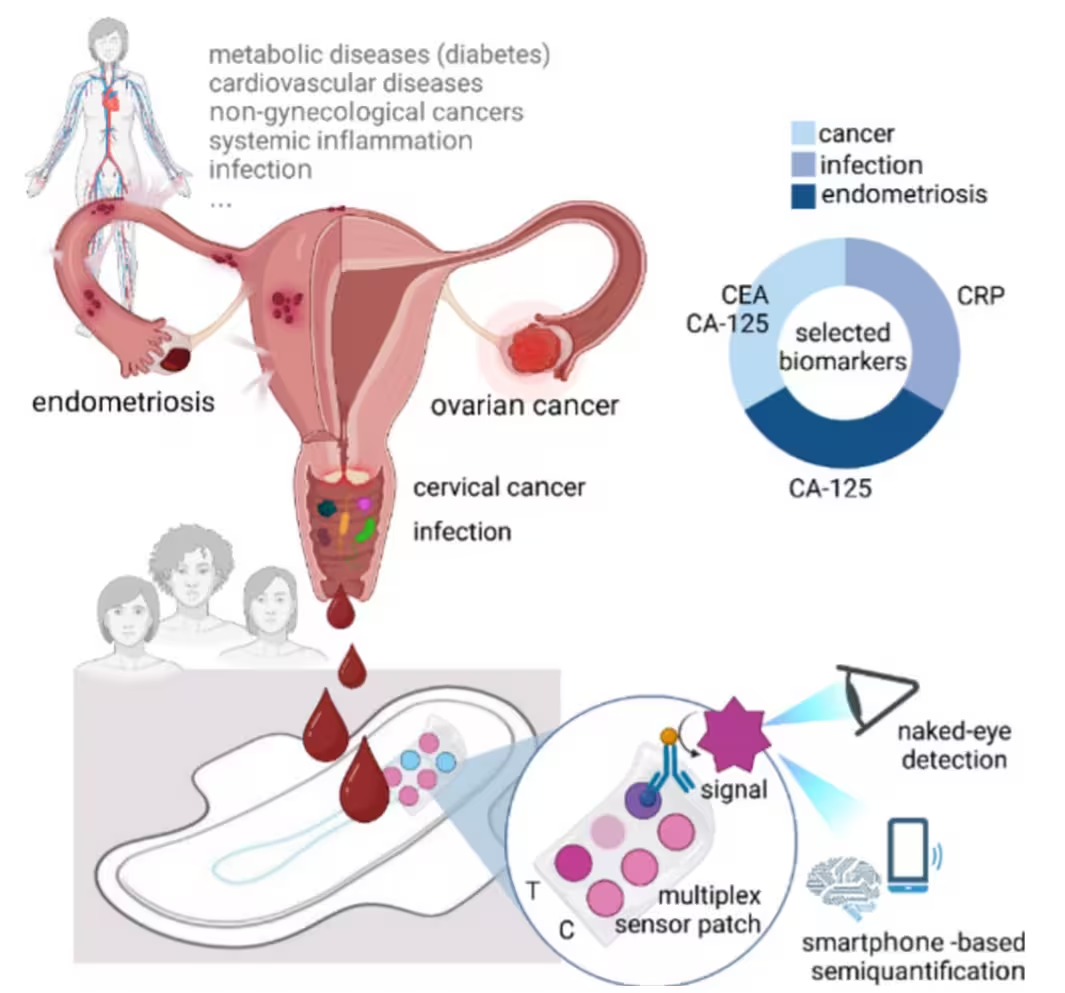
Every month, roughly 1.8 billion people of reproductive age menstruate, producing a biological sample that has been largely treated as waste. Like venous blood, menstrual blood contains proteins, immune markers and other molecular biomarkers that can reveal information about reproductive health, infections, inflammatory conditions and—potentially—early signals of cancer. Historically, menstrual sampling has been used mainly for fertility tracking; now, engineers and clinicians are exploring its wider diagnostic potential with low-cost, point-of-care technologies.
MenstruAI: a wearable microfluidic sensor for pads
Researchers led by Inge Herrmann at ETH Zurich developed a paper-based microfluidic platform called "MenstruAI" that integrates into a standard sanitary pad. MenstruAI is a lateral flow, colorimetric assay built on antibody-functionalized gold nanoparticles. Different test zones on the paper strip are tailored to bind biomarkers associated with conditions such as endometriosis, infections or cancer. When menstrual fluid reaches a test zone, nanoparticle binding produces a visible colour change, enabling naked-eye detection.
How the platform works
- The pad channels menstrual fluid into paper microfluidic lanes.
- Antibody-coated gold nanoparticles in each lane capture target proteins or antigens.
- Specific binding produces a colorimetric signal; intensity correlates with biomarker abundance.
To simplify result reading and reduce user bias, the ETH team paired the strip with a smartphone application. The app walks users through image capture, then applies machine learning models trained on hundreds of labelled test-strip images to interpret colour patterns and provide a preliminary assessment.
Advantages, context and potential impact
MenstruAI avoids the pre-processing (centrifugation, pipetting) common to many laboratory assays: menstrual fluid is applied directly and analysed without additional sample handling. This non-invasive, low-cost approach was explicitly designed to be "accessible, affordable, reproducible, [and] non-invasive," making it especially valuable where clinical access is limited by geography or economic constraints. Key keywords for uptake include point-of-care diagnostics, wearable diagnostics, menstrual blood biomarkers, and microfluidics.
The team frames MenstruAI as a screening and monitoring tool—not a substitute for clinical lab tests. As a low-barrier early-warning system, it could encourage timely medical follow-up and expand preventive care for populations with limited access to routine check-ups.
Next steps and research needs
The published work is a proof-of-concept. Larger field trials are needed to map biomarker variability across age groups, menstrual phases and populations, and to validate sensitivity and specificity versus standard clinical assays. Researchers also aim to broaden the panel to include sexually transmitted infection markers or additional inflammatory indicators.
Expert Insight
"Turning routine menstrual flow into a diagnostic window is both scientifically intriguing and socially significant," says Dr. Maya Thompson, fictional biomedical engineer and science communicator. "The technical challenge is controlling variability—volume, cycle phase and contamination—while ensuring robust machine-learning interpretation. If validated at scale, such wearables could change how we think about preventive care for reproductive health."
Conclusion
MenstruAI demonstrates how a simple wearable—integrating paper microfluidics, antibody-functionalized gold nanoparticles and smartphone machine learning—can transform menstrual blood from discarded material into a meaningful health resource. By combining non-invasive sampling, low-cost materials and digital interpretation, this approach could democratize access to early screening and ongoing monitoring for reproductive and systemic conditions, provided forthcoming field validation confirms clinical utility.
Source: advancedsciencenews

Leave a Comment