4 Minutes
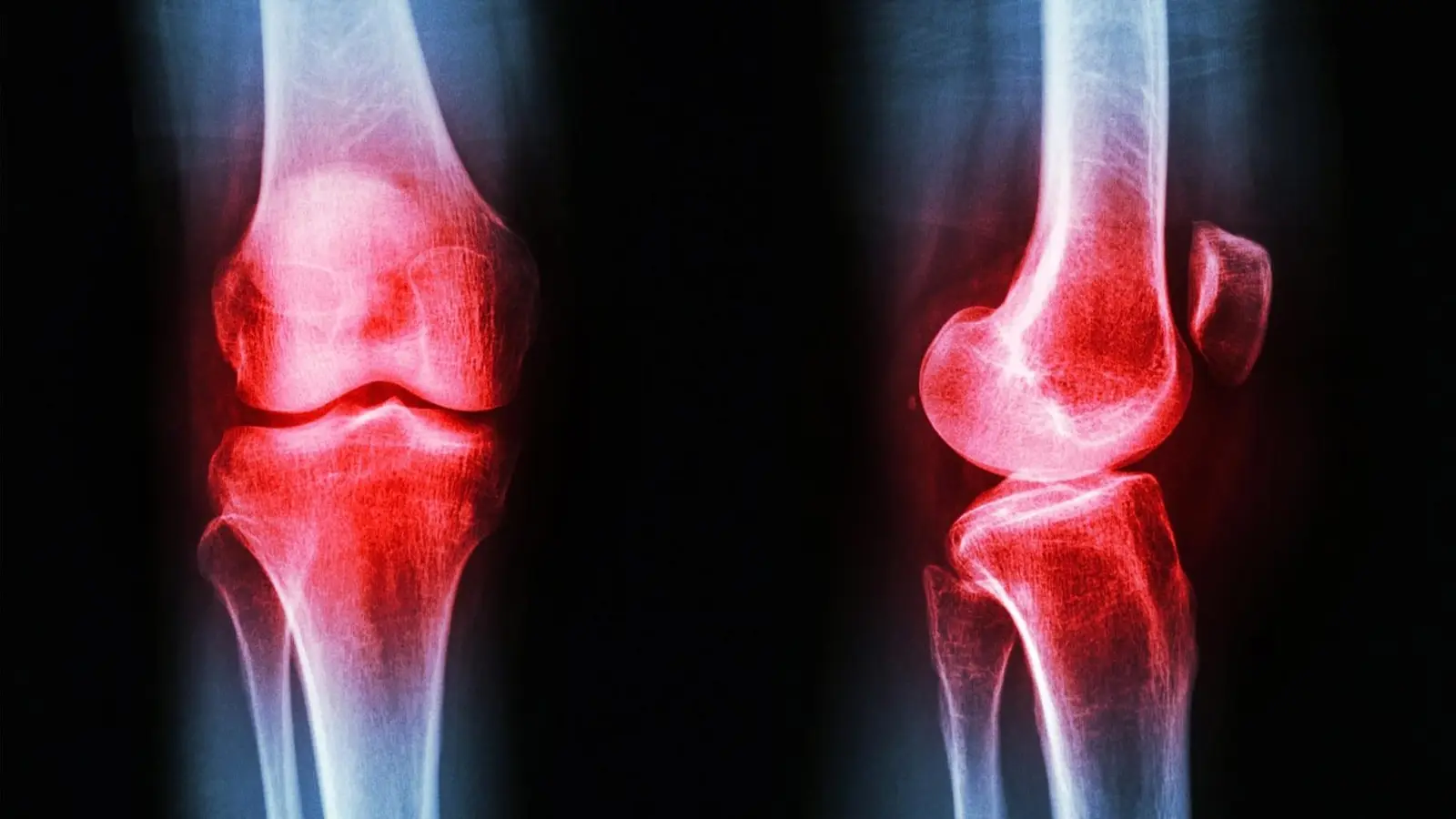
Lead researcher Scott Uhlrich measures a participant’s gait. At the beginning of the study, participants received a baseline MRI and walked on a force-sensitive treadmill while motion-capture cameras recorded their walking mechanics. Credit: Utah Movement Bioengineering Lab
Researchers have reported a non-pharmacological, low-risk approach to reduce knee osteoarthritis pain by changing how people walk. In a controlled trial, participants received individualized foot-angle prescriptions based on motion-capture analysis and force-sensitive treadmill data. Their progress was tracked with baseline and follow-up MRIs, objective gait measures, and self-reported pain scores.
Scientific background and experimental details
Osteoarthritis is a degenerative joint condition characterized by cartilage breakdown, pain, and reduced mobility. Conventional management includes medications (from over-the-counter analgesics to prescription opioids), lifestyle modification, and ultimately joint replacement for advanced disease. The new study tests gait retraining — a behavioral intervention that alters foot placement and walking mechanics — to reduce joint loading and slow cartilage damage.
Participants in the trial underwent detailed biomechanical assessment using motion-capture cameras and a force-sensitive treadmill to quantify joint forces and foot angles. Investigators used those data to prescribe a personalized change in foot strike angle during walking and monitored adherence and outcomes with repeat MRIs and clinical pain scales.

Key findings and clinical implications
The intervention delivered clinically meaningful pain reduction compared with placebo. As lead researcher Scott Uhlrich summarized, "The reported decrease in pain over the placebo group was somewhere between what you’d expect from an over-the-counter medication, like ibuprofen, and a narcotic, like oxycontin." In addition, MRI analyses indicated slower deterioration in a measurable marker of cartilage health in the retraining group.
Beyond objective measures, participants reported high satisfaction. One participant commented: "I don’t have to take a drug or wear a device…it’s just a part of my body now that will be with me for the rest of my days, so that I’m thrilled with."
Advantages of a behavioral approach
Gait retraining is low-cost, non-invasive, and potentially durable. For people in their 30s to 50s, delaying or reducing the need for long-term pharmacologic pain management or premature joint replacement could represent a major public-health benefit. "Especially for people in their 30’s, 40’s, or 50’s, osteoarthritis could mean decades of pain management before they’re recommended for a joint replacement," Uhlrich said. "This intervention could help fill that large treatment gap."

Related technologies and path to clinical use
Currently, the foot-angle prescriptions were derived from lab-grade motion capture, which is costly and time-consuming. To scale this approach, researchers are exploring mobile sensor solutions: smartphone video analysis, wearable "smart shoes," and other inertial sensors that can personalize and deliver retraining in outpatient physical-therapy settings during ordinary walks. Further trials will be required to validate sensor-based prescriptions, confirm long-term adherence, and evaluate real-world effectiveness before broad clinical deployment.
Expert Insight
Dr. Maria Chen, a clinical biomechanics researcher not affiliated with the study, notes: "This work translates fundamental gait mechanics into a practical therapy. If mobile sensors can reliably reproduce lab measurements, gait retraining could become an accessible first-line strategy to manage early osteoarthritis and reduce reliance on medications. The next steps are robust validation and integration into routine physical therapy workflows."
Conclusion
This gait-retraining study suggests a promising, drug-free method to lessen knee osteoarthritis pain and slow cartilage decline. By combining biomechanical assessment with personalized walking prescriptions, the approach targets joint loading directly. Continued development of mobile sensor technologies and larger trials will determine whether this accessible intervention can be widely adopted to improve long-term outcomes for people with osteoarthritis.
Source: scitechdaily

Leave a Comment