6 Minutes
Sleep, the Brain, and Waste Clearance
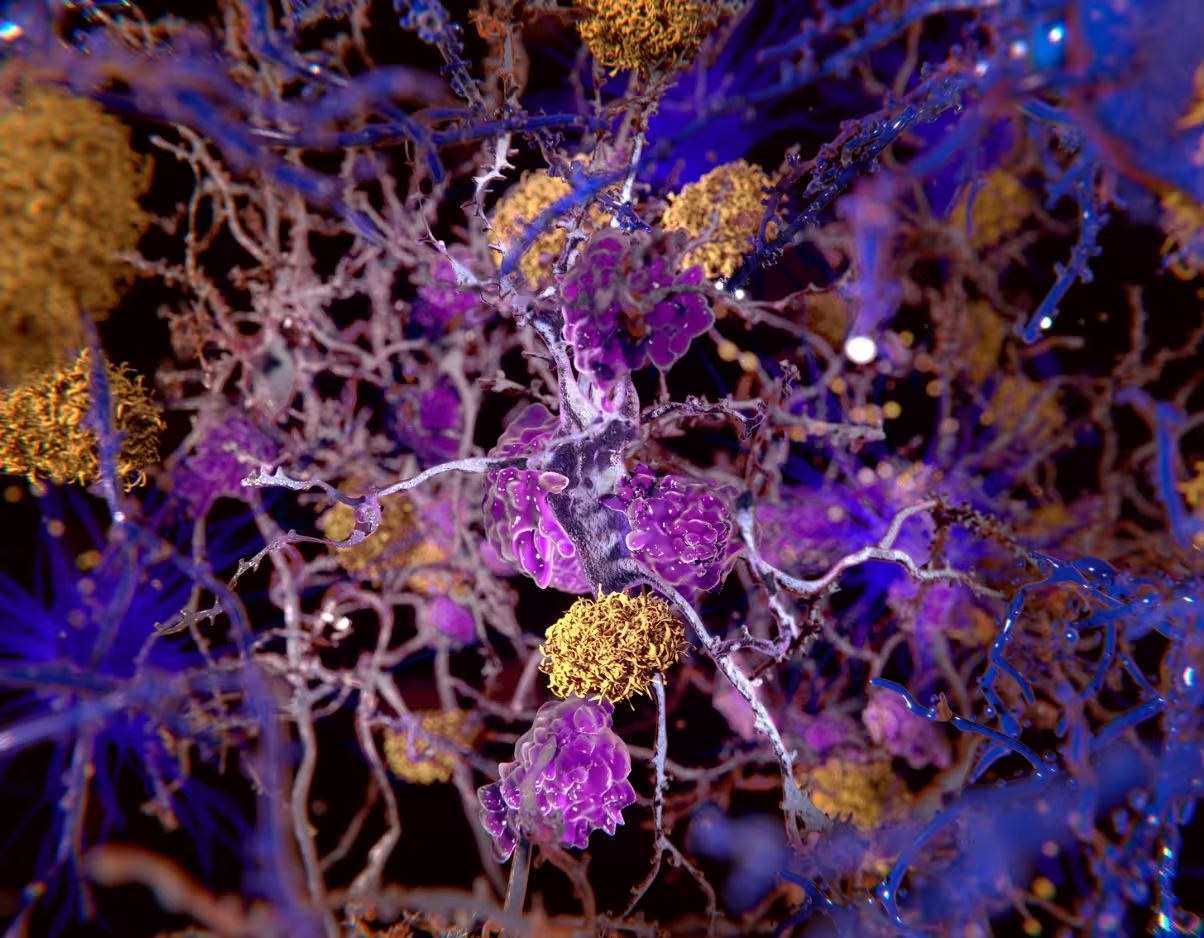
The brain appears to have a dedicated waste-removal network called the glymphatic system, which researchers propose is more active during sleep. This mechanism uses cerebrospinal fluid to wash through spaces around blood vessels and between brain cells, collecting metabolic byproducts and carrying them away via draining veins. (koto_feja/E+/Getty Images)
Emerging evidence suggests disrupted or insufficient sleep could impair this clearance process and allow neurotoxic proteins to accumulate — potentially increasing the risk of dementia. While much of the mechanistic work has been carried out in mice, growing human data indicate sleep quality influences levels of proteins linked to Alzheimer’s disease and other dementias.
Scientific background: How the glymphatic system works and why waste matters
The lymphatic system outside the brain clears cellular waste by moving fluid from intercellular spaces into the bloodstream. The brain, however, lacks classical lymphatic vessels. About a decade ago scientists described the glymphatic system as a brain-specific clearance route driven by cerebrospinal fluid (CSF) flow.
CSF circulates around the brain and spinal cord, flows into perivascular spaces surrounding arteries, moves into interstitial spaces between neurons and glial cells, picks up metabolites and proteins, then exits along perivenous pathways and meningeal lymphatic channels. Key waste products of interest for dementia researchers include amyloid beta (Aβ) and tau proteins. When Aβ aggregates into plaques and tau forms tangles inside neurons, they are central pathological hallmarks of Alzheimer’s disease.
Studies in rodents reported increased glymphatic activity during sleep, with more robust CSF circulation and faster removal of Aβ. Multiple human studies have found Aβ concentrations in CSF and certain brain regions rise during wakefulness and decline across sleep, supporting a sleep-dependent clearance model — though some recent animal work has produced conflicting timing results, underlining ongoing debate about daily rhythms of glymphatic flow.
Evidence in humans: sleep deprivation and protein clearance
Human experiments show short-term sleep loss can affect biomarkers associated with dementia. For example, a single night of total sleep deprivation in healthy adults raised Aβ levels in the hippocampus, a memory-related structure vulnerable in early Alzheimer’s disease. These results suggest sleep influences how Aβ is cleared from the human brain, consistent with glymphatic hypotheses derived from animal models.
However, translating animal physiology into human clinical recommendations remains challenging. Differences in brain size, posture, vascular dynamics, and sleep architecture mean mechanisms observed in mice may not map directly onto people. Still, epidemiological studies consistently link chronic poor sleep with worse cognitive outcomes across the lifespan.
Sleep disorders: sleep apnoea, insomnia and dementia risk
Two common disruptions to sleep are sleep apnoea and chronic insomnia. Obstructive sleep apnoea causes repeated breathing pauses during sleep, fragmenting sleep and lowering blood oxygen. These effects can produce chronic sleep deprivation and vascular stress, both potential contributors to protein accumulation in the brain. Observational studies report higher dementia risk among people with untreated sleep apnoea, and some studies show improved removal of Aβ after patients receive effective therapy such as continuous positive airway pressure (CPAP).
Insomnia — difficulty falling or staying asleep — is also associated with increased dementia risk when it is long-standing. Yet evidence that treating insomnia reduces levels of dementia-linked proteins is currently limited. Clinical trials are underway to test whether targeted therapies, including cognitive-behavioural therapy for insomnia and pharmacological approaches like orexin receptor antagonists, alter biomarkers such as Aβ and tau.
Ongoing research, methods and implications for prevention
Researchers are expanding methods to monitor brain waste clearance noninvasively. Studies measure Aβ and tau in blood and CSF across the 24-hour sleep–wake cycle, or before and after sleep-disrupting interventions. Clinical trials are evaluating whether treating sleep apnoea improves biomarker trajectories and whether sleep-focused interventions can be protective against cognitive decline.
If confirmed, sleep improvement would be a broadly accessible strategy for dementia risk reduction, complementing lifestyle measures such as cardiovascular health, exercise, and diet. Potential future tools include sleep-targeted drugs, optimized sleep hygiene programs, and wearable technologies that track sleep quality and timing to identify people at risk.
Expert Insight
Dr. Elena Moreno, a sleep neurologist and research fellow, comments: 'The convergence of sleep science and neurodegeneration research is one of the most promising areas for near-term preventive strategies. While causality is not yet established, improving sleep is low-risk and offers many cognitive and cardiovascular benefits. We need larger longitudinal trials to show whether improving sleep actually slows protein accumulation and clinical decline.'
Conclusion
Current data support the idea that sleep plays an important role in clearing brain waste, including amyloid beta and tau proteins linked to Alzheimer’s disease. Although animal studies strongly implicate the glymphatic system, human research is still clarifying timing, mechanisms and therapeutic potential. Treating sleep disorders such as sleep apnoea appears beneficial for overall brain health, but more trials are required to prove that improving sleep directly reduces dementia incidence. If you are worried about your sleep or cognitive function, consult your physician for assessment and evidence-based treatment options.
Source: sciencealert

Leave a Comment