5 Minutes
Researchers have identified a previously unrecognized immune pathway in the intestine that drives life-threatening food allergy reactions. Rather than the well-known mediator histamine, a class of lipid signaling molecules called cysteinyl leukotrienes appears to power severe gastrointestinal anaphylaxis. The discovery — led by teams at Arizona State University in collaboration with Yale and other partners and published in Science — points to existing asthma drugs as potential tools to prevent or lessen food-induced anaphylactic episodes.
Scientific background: mast cells, IgE and chemical mediators
Food allergy develops when the immune system erroneously treats a dietary protein as hazardous. Key players are mast cells, a type of immune cell loaded with preformed and newly synthesized mediators. When mast cells detect allergens bound to immunoglobulin E (IgE) antibodies, they activate and release compounds that alter blood vessel tone, mucus secretion and smooth-muscle contraction. In systemic or injected-allergen reactions, histamine is the dominant mediator and antihistamines can be partially effective.
However, the intestine hosts distinct mast cell populations that behave differently. The new research shows intestinal mast cells receive cues from nearby epithelial cells that bias them toward producing leukotrienes — potent inflammatory lipids that constrict airways, boost vascular permeability and amplify inflammation. Because leukotrienes are already implicated in asthma physiology, the finding links mechanisms across respiratory and gastrointestinal allergic disease.
Study design and key findings
The investigators combined genetic, cellular and pharmacological approaches in preclinical models to compare allergic responses triggered by ingested versus injected allergens. They found that after oral exposure, intestinal mast cells produced relatively little histamine and instead produced elevated levels of cysteinyl leukotrienes. Detailed transcriptional and biochemical profiling revealed that gut mast cells are a distinct subtype primed for leukotriene biosynthesis.
To test causality, the team used zileuton — an FDA-approved 5-lipoxygenase inhibitor prescribed for certain asthma patients — to block leukotriene synthesis. Zileuton reduced clinical signs of food-triggered anaphylaxis and prevented the characteristic hypothermic response in the models. Crucially, the drug did not prevent reactions induced by allergens injected directly into the bloodstream, demonstrating that gut-initiated anaphylaxis operates through a different chemical pathway than systemic anaphylaxis.
Clinical implications and translational prospects
Current emergency treatment for severe anaphylaxis centers on intramuscular epinephrine to reverse acute cardiovascular and airway collapse. Antihistamines have limited preventive value for severe food reactions. The new results suggest that therapies targeting leukotriene production (e.g., zileuton) or leukotriene receptors (e.g., montelukast) could become adjunctive or preventive treatments specifically for food-triggered anaphylaxis. Because these drugs are already approved for asthma, repurposing could accelerate clinical testing. Still, the authors emphasize that human studies are required to confirm whether the same mast cell subsets and leukotriene-dependent pathway exist in people with food allergy.
Broader implications for immunology and diagnostics
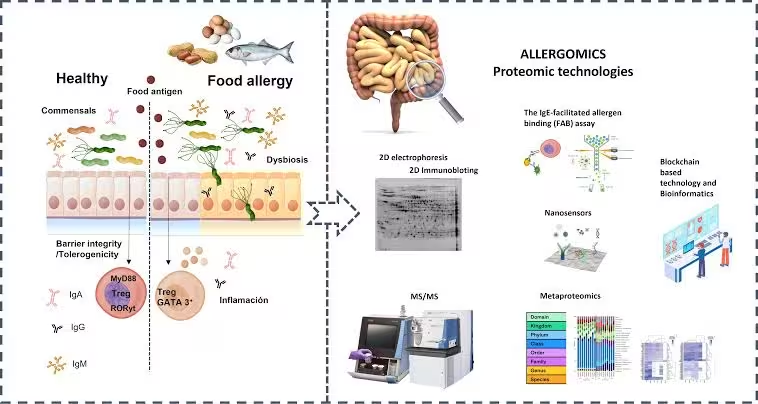
Beyond therapeutics, the study reframes how scientists interpret allergic risk and immune sensing. It demonstrates that the route of allergen entry — skin, bloodstream or gut — shapes which cell types and mediators dominate the response. This insight may explain why circulating levels of food-specific IgE do not reliably predict clinical severity: identical antibody signatures can produce different outcomes depending on tissue context and local cell programming. The finding also raises questions about how diet, the gut epithelium and the microbiome influence mast cell phenotypes.
Expert Insight
"This work underscores the importance of tissue context in immune responses," says Dr. Elena Moreno, an immunologist and clinical researcher (fictional) specializing in mucosal allergy. "If supported by human data, targeting leukotriene pathways could provide a much-needed strategy to reduce the frequency or severity of food-induced anaphylaxis — especially for people who remain at high risk despite avoidance and current therapies. Careful clinical trials will be essential to assess efficacy and safety when moving from animal models to patients."
Conclusion
The discovery of a leukotriene-driven pathway in intestinal mast cells changes the understanding of food-triggered anaphylaxis and opens a translational pathway using existing asthma medications. While promising, these findings require validation in human tissues and clinical trials. If confirmed, targeting leukotriene synthesis or signaling could become a new preventive or adjunctive strategy to protect people with life-threatening food allergies.
Source: sciencedaily

Leave a Comment