5 Minutes
Summary and key finding
Bacteria commonly resident in the human mouth have been detected inside atherosclerotic plaques in coronary arteries, and their presence is strongly associated with severe coronary disease and fatal heart attacks, according to a new study led by researchers at Tampere University in Finland. The research analyzed arterial plaques from over 200 patients with coronary artery disease and found DNA and structural evidence of oral microbes embedded within plaque cores, suggesting a potential direct role for oral bacteria in plaque destabilization and rupture.
Study design and scientific background
Atherosclerosis—the progressive accumulation of fat, cholesterol, calcium and cellular debris on artery walls—remains a principal cause of myocardial infarction (heart attack). For decades, epidemiological studies have linked poor oral health and periodontal disease with higher cardiovascular risk, but a clear mechanistic connection has been elusive.
To investigate whether oral microbes colonize coronary plaques, the research team collected coronary atheromas from two groups: 121 individuals who suffered sudden death and 96 patients who underwent surgery to remove obstructive plaques. The samples were examined using quantitative polymerase chain reaction (qPCR) to detect microbial DNA, immunohistochemistry to localize microbial proteins and toxins, and transcriptomics to measure microbial and host gene expression within the tissue.
These complementary molecular and histological techniques revealed bacterial biofilms—structured communities of microbes encased in protective extracellular matrix—embedded at the lipid core of many plaques. Viridans streptococci, a group of oral streptococci commonly found in dental biofilms and the oropharynx, were the single most frequently detected lineage, present in roughly 42% of plaques in both sample sets (42.1% of sudden-death plaques; 42.9% of surgical plaques).
Findings, interpretation and potential mechanisms
Microscopic images and molecular signatures indicated that bacterial biofilms were localized deep within plaque cores, potentially sheltered from normal immune surveillance. The investigators report a strong correlation between the presence of oral bacteria and clinical outcomes: advanced atherosclerosis, death due to cardiovascular disease, and myocardial infarction—especially cases associated with plaque rupture.
The proposed mechanism is that dormant bacterial biofilms residing in the plaque can remain clinically silent until a secondary stressor—such as systemic infection, respiratory viruses, metabolic changes from diet, or surges in stress hormones like norepinephrine—induces local inflammation. That inflammation could weaken the fibrous cap or destabilize the lipid core, precipitating plaque rupture and acute coronary thrombosis.
As the study authors state, "The change from a stable soft‐core coronary atheroma into a vulnerable rupture‐prone coronary plaque may be contributed to by a chronic bacterial infection in the form of a dormant biofilm that colonizes the lipid core and wall of the atheroma and evades immune detection." The work opens avenues for diagnostics and prevention focused on microbial drivers of plaque vulnerability.
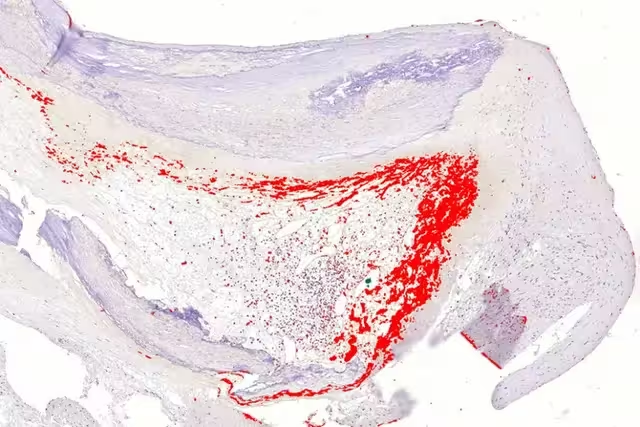
A bacterial biofilm (red) found inside a coronary artery plaque. (Pekka Karhunen's research group/Tampere University)
Implications for prevention, diagnostics and future research
If replicated and extended, these findings could reshape cardiovascular prevention strategies by integrating oral microbiology and antimicrobial or biofilm-targeted approaches into risk assessment. Future studies must answer critical questions: how do oral microbes translocate from the mouth to arterial tissue; which species or strains are most pathogenic in plaques; what host factors permit biofilm persistence; and which triggers convert dormant biofilms into active, inflammatory lesions.
Diagnostics might evolve to include molecular screening of circulating bacterial DNA or biomarkers of biofilm activity, while preventive interventions could emphasize improved oral hygiene, periodontal treatment, and targeted antimicrobial or anti-biofilm therapies. Importantly, the study reinforces the public-health message that oral health is integral to cardiovascular health.
Expert Insight
Dr. Emma Rhodes, a cardiovascular microbiome researcher (fictional), comments: "This study provides compelling molecular evidence that oral microbes can inhabit plaque cores. While causality needs further work, the data suggest we should treat oral infections as a modifiable cardiovascular risk factor. Future randomized trials testing periodontal treatment and biofilm-directed therapies will be essential to determine clinical benefit."
Her perspective underscores a pragmatic path forward: integrate dental care into cardiovascular risk management and pursue translational work to move from association to intervention.
Conclusion
The Tampere University study adds significant molecular and histological evidence linking oral bacteria—particularly viridans streptococci—to vulnerable coronary plaques and fatal heart attacks. By identifying dormant bacterial biofilms at the heart of atherosclerotic lesions, the research highlights a potentially actionable intersection between dental health, microbiology, and cardiology. Further research is needed to confirm causation, map transmission pathways, and evaluate preventive or therapeutic strategies that target microbial biofilms to reduce the burden of acute coronary events.
Source: sciencealert


Leave a Comment