5 Minutes
Non-invasive stool test approaches colonoscopy accuracy
A research team at the University of Geneva (UNIGE) has developed a machine-learning approach that analyzes the human gut microbiome at the subspecies level and can identify colorectal cancer from stool samples with about 90% sensitivity. Published in Cell Host & Microbe, the study presents the first comprehensive catalogue of gut bacterial subspecies and uses it to build predictive models that nearly match colonoscopy performance while offering a low-cost, non-invasive screening alternative.
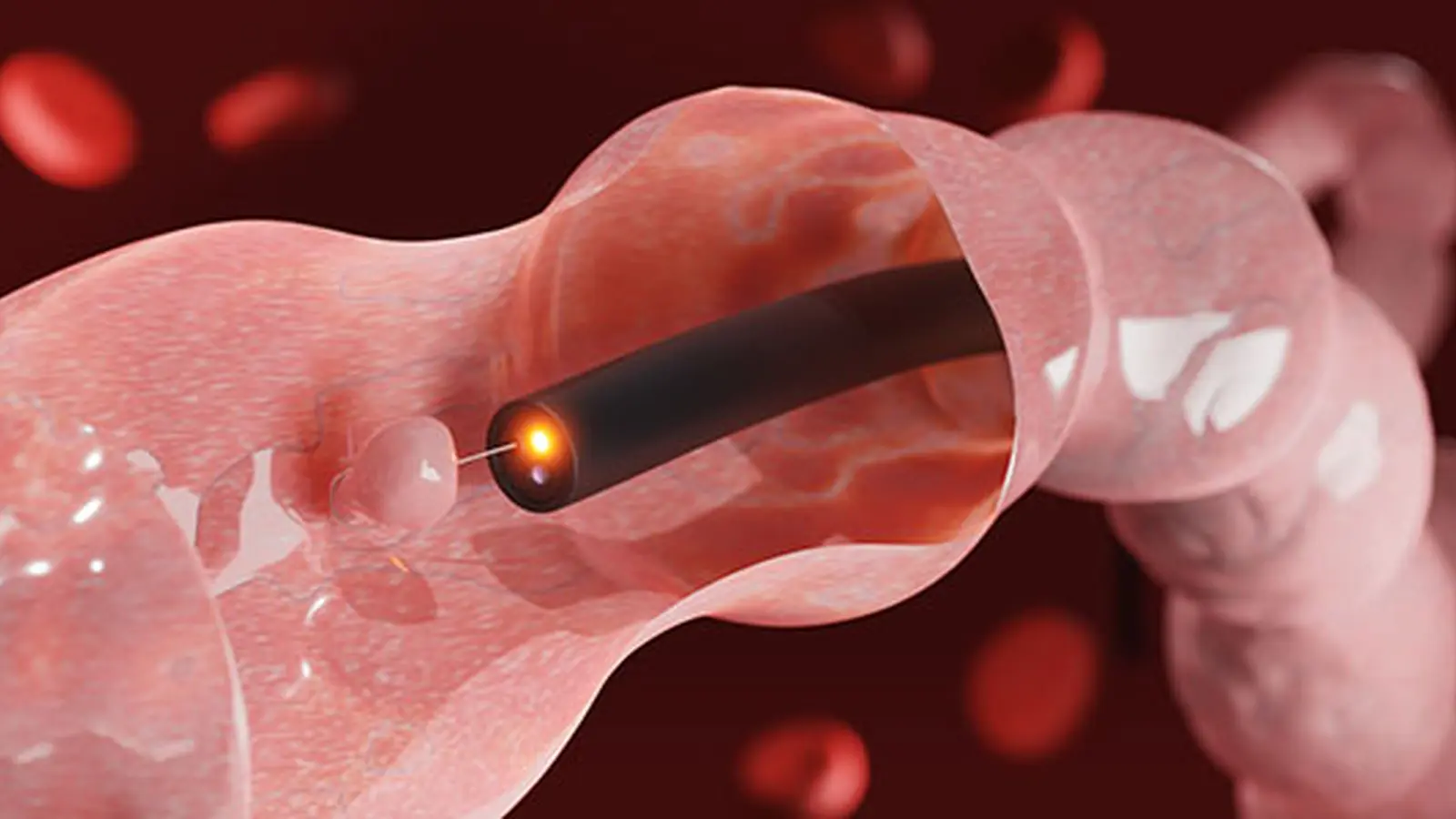
Colorectal cancer is one of the world’s leading causes of cancer mortality, and early detection dramatically improves treatment outcomes. However, colonoscopies—the clinical gold standard—are costly, resource intensive and often avoided because of discomfort and preparation burdens. A high-performing stool test based on microbiome signatures could increase screening uptake, detect cancers earlier, and triage who needs confirmatory colonoscopy.
Scientific background: subspecies resolution and why it matters
Subspecies resolution explained
Bacterial taxonomy is commonly reported at the species or strain level. Species-level analysis can miss functional differences among genetically distinct subgroups, while strain-level signatures vary widely between individuals and populations. The UNIGE team focused on an intermediate taxonomic level—subspecies—to capture consistent biological differences that influence host physiology across diverse cohorts.
Using large-scale metagenomic datasets, bioinformaticians reconstructed an atlas of gut microbiome subspecies. This finer resolution allowed researchers to distinguish microbial subgroups with divergent roles in inflammation, metabolism and tumor biology—differences that are invisible in coarser analyses but reproducible enough to train robust machine-learning classifiers.
Methods, key findings and clinical implications
The group combined their subspecies catalogue with clinical metadata and developed algorithms to classify stool samples as cancer-positive or negative. Matija Trickovic, the study’s first author, described the computational challenge of parsing massive datasets and said the team implemented a precise pipeline suitable for both research and clinical use. The model detected approximately 90% of colorectal cancer cases in validation sets—close to the 94% detection rate reported for colonoscopy and superior to existing non-invasive tests.

Lead investigator Mirko Trajkovski emphasized that subspecies-level mapping captures functional variation among bacteria that can either promote or inhibit tumor development. By focusing on reproducible subspecies signatures rather than broadly defined species or highly individualized strains, the model generalizes across different populations and geographic regions.
A clinical trial is planned with Geneva University Hospitals (HUG) to evaluate the test across cancer stages and lesion types. In a possible screening workflow, positive microbiome results would be followed by targeted colonoscopy, reducing the number of full colonoscopies needed and enabling earlier intervention for cancers that would otherwise be missed.
Beyond colorectal cancer, the approach opens avenues for non-invasive diagnostics of other cancers and chronic diseases where the gut microbiota plays a role. Mapping subspecies differences could also reveal mechanisms by which microbes affect inflammation, immune responses and drug metabolism, informing personalized therapies.
Expert Insight
Dr. Laura Chen, clinical microbiologist and science communicator, comments: "This study shows the value of resolving the microbiome at a level that is both biologically meaningful and clinically useful. Machine learning applied to a robust subspecies catalogue can extract signals that simpler tests miss. The next steps—large multicenter trials and integration with clinical workflows—will determine how rapidly this technology can improve screening programs worldwide."
Operational challenges remain: standardizing stool collection, ensuring reproducible sequencing across labs, and validating performance in screening populations that include asymptomatic people and younger adults, where incidence is rising. Integrating more clinical and demographic data could further refine accuracy and reduce false positives.
Conclusion
UNIGE’s subspecies-level gut microbiome atlas and AI classifiers present a promising non-invasive method to detect colorectal cancer with near-colonoscopy sensitivity. If validated in broader clinical trials, stool-based microbiome screening could increase early detection, reduce reliance on invasive procedures, and extend to diagnostics for other diseases influenced by the microbiota. This approach highlights how high-resolution microbiome mapping combined with machine learning can translate microbial ecology into actionable clinical tools.
Source: sciencedaily

Leave a Comment