5 Minutes
Stem cell injections reverse stroke damage in mouse brains
Researchers from the University of Zurich and the University of Southern California report that transplanted human stem cells can repair brain tissue damaged by ischemic stroke in mice. In a preclinical model, injected stem cells survived, matured into neuron-like cells, and formed connections with host tissue. The study, published in Nature Communications, suggests a multi-faceted regenerative response: neural differentiation, vascular repair, reduced inflammation, and strengthened blood-brain barrier integrity. These outcomes were accompanied by measurable improvements in motor coordination in treated animals.
Scientific background and experimental approach
Stroke—caused by internal bleeding or oxygen restriction when blood vessels are blocked—kills brain cells and often produces lasting deficits in speech, movement, and cognition. Current therapies focus on limiting acute damage and rehabilitation; regenerative approaches aim instead to replace or restore lost neural tissue. In this study, researchers used mice with stroke-induced lesions and injected human neural stem cells into the affected brain regions once the acute phase had stabilized. The timing of transplantation is critical: prior work by the team established that the brain must reach a certain stabilization window after stroke for engraftment to be effective.
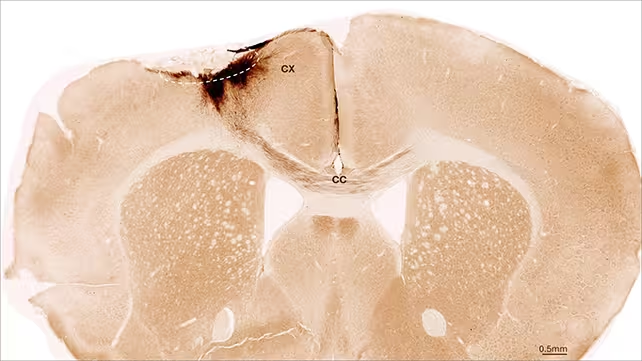
Using immunohistochemistry and functional assays over a five-week follow-up, the team tracked the implanted cells. Most of the transplanted cells remained localized, developed morphological and molecular hallmarks of immature neurons, and extended projections that made contact with resident neurons and local circuits. The investigators also documented concurrent vascular remodeling—blood vessels showed signs of self-repair—alongside reduced markers of inflammation and an improvement in blood-brain barrier properties, which together create an environment more permissive for recovery.
Key discoveries and implications for stroke recovery
The primary findings are threefold: first, implanted human neural stem cells can survive and differentiate into neuron-like cells in a damaged adult brain; second, these cells can integrate structurally and form synaptic contacts with host tissue; third, stem cell transplantation appears to trigger secondary regenerative processes such as angiogenesis (blood-vessel repair) and immune modulation. Functionally, treated mice demonstrated better motor performance than controls—an essential translational signal because motor deficits are among the most debilitating outcomes of stroke.
These results reinforce the concept that cell-based therapies could one day restore functions currently considered irreversible. They also highlight the importance of combining measures of cell survival with assessments of connectivity, vascular health, inflammation, and behavior when evaluating regenerative strategies for the central nervous system.
Challenges, safety and path to clinical translation
Despite promising preclinical data, several obstacles remain before human application. Long-term safety must be demonstrated: implanted cells should not proliferate uncontrollably or migrate beyond intended targets. The optimal delivery route, dosing, and timing windows require refinement. Immune compatibility and scaling from mouse brains to the human brain’s larger, more complex architecture also present major translational hurdles. Finally, regulatory pathways for stem cell products demand rigorous, multi-year safety and efficacy trials.
The research team emphasizes caution and measured optimism. According to lead investigators, their analyses go beyond immediate post-transplant effects to evaluate whether newly derived cells actually form neurological connections—an essential criterion for meaningful recovery.
Expert Insight
Dr. Maria Alvarez, a fictional neuroregeneration specialist, comments: 'This study is significant because it documents not only cell survival but also integration and collateral tissue repair. That combination—neurogenesis plus vascular and immune modulation—may be essential for durable functional recovery. Nevertheless, translating these results will require addressing immune rejection, long-term monitoring, and ensuring transplanted cells remain functionally appropriate in human circuitry.'
Conclusion
This study provides robust preclinical evidence that human neural stem cells can engraft, differentiate, and promote repair processes in stroke-damaged mouse brains. Findings include neuronal integration, vascular self-repair, reduced inflammation, and improved motor outcomes. While promising for future stroke therapies, translation to humans will require extended safety studies, optimization of timing and delivery, and careful clinical testing. The research adds an important chapter to regenerative neurology and underscores how combined cellular and tissue-level repair mechanisms might one day restore functions lost to stroke.
Source: sciencealert

Leave a Comment