5 Minutes
New analysis links A1 blood subgroup with higher early stroke risk
A large genetic analysis published in 2022 found that people whose genomes code for the A1 blood subgroup face a modestly increased risk of ischemic stroke before age 60. The study pooled data from multiple international cohorts and compared roughly 17,000 people who had experienced a stroke between ages 18 and 59 with nearly 600,000 stroke-free controls, identifying a reproducible signal near the genes that determine ABO blood groups.
Study design and key results
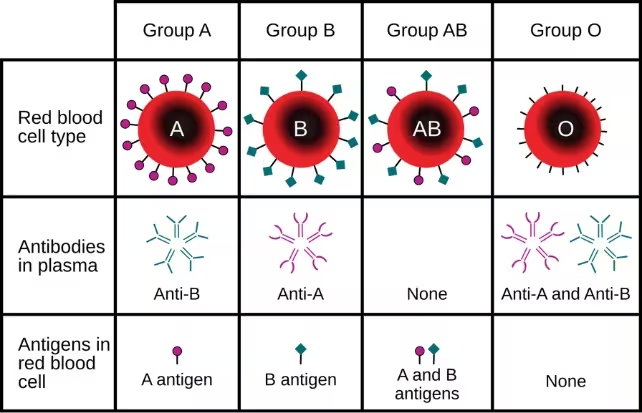
Researchers combined data from 48 genetic studies spanning North America, Europe, Japan, Pakistan and Australia. All participants in the primary analysis were aged 18–59. A genome-wide search highlighted two genomic regions associated with earlier stroke onset; one of these regions coincides with the ABO blood-group locus, which encodes the molecular markers on red blood cells that define types A, B, AB and O. Blood type is partly determined by the ABO blood group antigens present on red blood cells.
Targeted analyses of ABO variants showed that individuals whose DNA indicates the A subgroup variant A1 had about a 16% higher risk of having a stroke before age 60 compared with people with other ABO genotypes. By contrast, people carrying the O1 genotype showed an approximately 12% lower early-stroke risk. The authors emphasized that these relative risks are modest: in absolute terms the increased probability for any one person remains small.
The investigators also compared genetic associations in early-onset stroke (<60 years) with a dataset of older stroke cases (over age 60). The relationship between the A subgroup and stroke weakened and became non-significant in the late-onset group, suggesting different biological drivers for early- versus late-onset strokes.
Biological context and possible mechanisms
ABO locus, clotting and vascular biology
The ABO blood-group locus has been linked previously to coronary artery calcification, myocardial infarction and venous thromboembolism (blood clots in veins). Laboratory and epidemiological evidence indicate that ABO variants can influence circulating levels of clotting factors, platelet interactions and the function of endothelial cells that line blood vessels. These pathways are biologically plausible mechanisms by which an A-type genotype could slightly increase the propensity for clot formation, and thus ischemic stroke, especially in younger adults where atherosclerotic plaque buildup is less often the primary cause.
Despite these plausible links, the study's senior author, vascular neurologist Steven Kittner from the University of Maryland, cautioned that the precise mechanism remains unclear: 'We still don't know why blood type A would confer a higher risk,' he said. 'But it likely has something to do with blood-clotting factors like platelets and cells that line the blood vessels as well as other circulating proteins, all of which play a role in the development of blood clots.'
Limitations, population diversity and public-health context
Although the pooled sample was large, only about 35% of participants were of non-European ancestry, so the findings need replication in more diverse populations. Stroke incidence is also strongly age-dependent: in the United States nearly 800,000 people suffer a stroke each year, and about three-quarters of those events occur in people aged 65 and older. Stroke risk roughly doubles every decade after age 55, which helps put a 16% relative increase in younger adults into perspective — the absolute risk for most individuals remains low.
The study authors therefore do not recommend extra screening or heightened medical surveillance for people solely on the basis of their ABO blood type. Instead, they call for additional research to clarify the mechanisms linking ABO variants with clotting and to evaluate whether blood-type information could ever refine individualized risk prediction alongside other genetic and clinical markers.
Expert Insight
Dr. Maria Santos, a vascular epidemiologist at a university medical centre, commented on the study's implications: 'This work is important because it highlights how common genetic variation can subtly shift risk profiles for serious conditions like stroke. For clinicians, the practical message is unchanged: focus remains on controlling blood pressure, diabetes, smoking cessation and other modifiable risks. For researchers, the finding points to coagulation and vascular biology as areas needing more functional study to determine if targeted prevention strategies could emerge.'
Conclusion
The 2022 genetic meta-analysis strengthens evidence that inherited variation at the ABO blood-group locus, specifically the A1 subgroup, is associated with a modestly higher risk of ischemic stroke before age 60, while O1 appears modestly protective. The effect sizes are small and do not warrant changes to clinical screening based solely on blood type. Future studies with broader ancestry representation and laboratory work to test biological mechanisms are needed to determine whether ABO genotype can contribute meaningfully to personalized stroke prevention strategies.
Source: sciencealert


Leave a Comment