5 Minutes
Overview and key finding
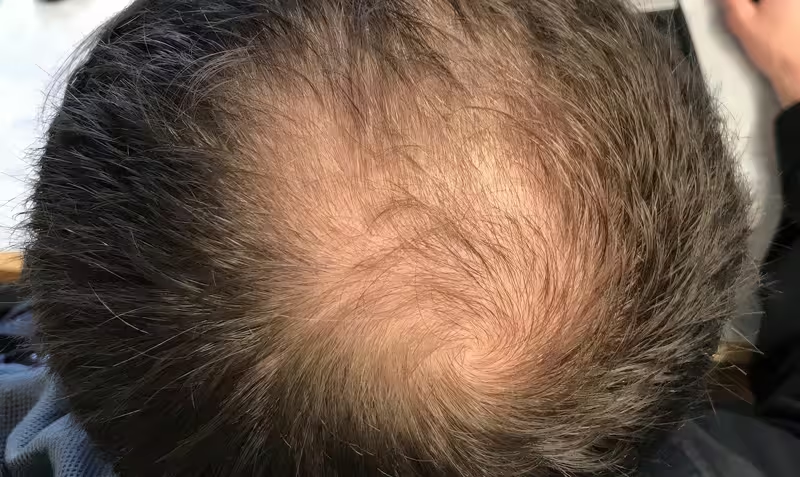
A new review of published research raises serious concerns about the psychiatric safety of finasteride, a widely prescribed drug for male pattern hair loss and benign prostatic hyperplasia (BPH). The analysis—covering eight studies published between 2017 and 2023 and drawing on multiple national data sources—finds consistent associations between finasteride use and elevated rates of mood disorders, suicidal ideation, and suicide. The review's author, Mayer Brezis, a retired nephrologist and former medical professor at Hadassah-Hebrew University Medical Center, argues that these signals have not received adequate attention from manufacturers or regulators, with potentially tragic public-health consequences.
Scientific background and mechanism
Finasteride acts by inhibiting 5-alpha-reductase, the enzyme that converts testosterone into dihydrotestosterone (DHT). Lowering DHT reduces male pattern hair loss and prostate enlargement, which explains the drug's clinical use since the 1990s. However, 5-alpha-reductase also catalyzes the formation of neurosteroids—such as allopregnanolone—that modulate GABAergic signaling and are implicated in mood regulation.
Animal studies suggest finasteride can trigger long-lasting brain changes, including hippocampal structural alterations and neuroinflammatory responses linked to anxiety and depression-like behaviors. Clinically, some patients report persistent psychiatric symptoms after stopping treatment—a phenomenon often referred to as post-finasteride syndrome. Post-finasteride syndrome is characterized by ongoing sexual dysfunction, cognitive complaints, and mood disturbances lasting months to years after drug discontinuation.
Regulatory history and reporting gaps
Regulators have been aware of mood-related signals for years. The U.S. Food and Drug Administration (FDA) added depression to finasteride’s label in 2011 and included suicidality in 2022. Internal FDA documents cited by Brezis indicate that agency experts recommended adding explicit warnings about ‘‘suicidal thoughts and behavior’’ as early as 2010; according to the review, that advice was not transparently disclosed at the time.
Brezis argues the low number of officially recorded suicides associated with finasteride (for example, 18 by 2011 in FDA reports) likely reflects broad underreporting and systemic pharmacovigilance failures rather than true absence of harm. He attributes part of the oversight to Merck and to regulators who did not require or perform robust database analyses that could have quantified risk more accurately. Merck has stated that available evidence does not support a causal link and that the company cooperates with regulators to analyze potential safety signals.
Data synthesis and implications for public health
The reviewed studies include cohort and case-control designs from several countries and consistently show higher incidence of mood disorders and suicidal ideation among finasteride users versus matched non-users. While observational research cannot prove causation, the cross-study coherence, biological plausibility (neurosteroid depletion and hippocampal effects), and reports of persistent symptoms strengthen the concern.
If the review’s extrapolations are accurate, the number of affected patients globally could be orders of magnitude higher than spontaneous reports suggest. That discrepancy highlights limitations in passive adverse-event reporting systems and points to the need for proactive post-approval safety research.
Recommendations for regulators and manufacturers
Brezis concludes that the regulatory framework should mandate ongoing post-approval analytical studies for drugs with widespread use and potential systemic effects on the brain. Key recommendations in the review include:
- Requiring manufacturers to commit, before approval, to periodic pharmacoepidemiologic analyses and to make results public.
- Empowering regulators to conduct independent database assessments when safety signals emerge.
- Updating product labels and patient information with clear language about psychiatric risks and the potential for persistent symptoms after discontinuation.
These measures aim to balance innovation with patient safety and to reduce conflicts of interest that can hinder transparent risk assessment.
Clinical context and patient guidance
For clinicians and patients, the review reinforces the importance of informed consent. Prescribers should discuss psychiatric risks when recommending finasteride, especially to individuals with a personal or family history of mood disorders. Monitoring for new or worsening depressive symptoms and suicidal ideation should be routine, and patients should be advised to report psychiatric side effects promptly.
Alternative hair-loss strategies, counseling about realistic expectations, or referral to dermatology or mental-health specialists may be appropriate when risks outweigh perceived benefits. Clinicians should also consider the small but non-negligible potential for prolonged adverse effects after stopping the drug.
Expert Insight
"The finasteride debate underscores a broader challenge in pharmacovigilance," says Dr. Laura Anders, a clinical pharmacologist and drug-safety specialist. "When a medication acts on enzymes that influence both peripheral tissue and central neurosteroids, early and sustained safety surveillance is essential. Passive reporting systems alone are insufficient; active database studies and transparent regulatory communication can help identify rare but serious outcomes sooner."
Conclusion
The review amplifies long-standing concerns that finasteride may carry psychiatric risks that have been underappreciated by regulators, manufacturers, and clinicians. Given the drug's biological mechanisms and consistent observational evidence, the study calls for stronger post-approval safety obligations, clearer patient communication, and more rigorous pharmacovigilance. For patients and prescribers, the take-home message is to weigh cosmetic benefits against potential long-term neuropsychiatric harms and to maintain vigilant monitoring when finasteride is used.
Source: sciencealert

Leave a Comment