6 Minutes
Psychedelics and Immune Control: A New Research Frontier
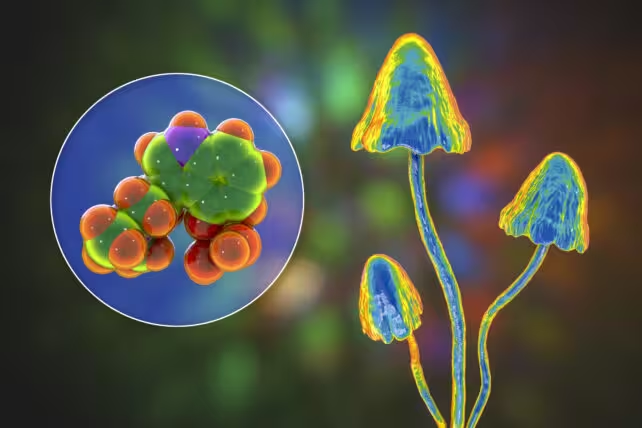
Psychedelic compounds once relegated to counterculture imagery are re-emerging as serious subjects of biomedical research. Beyond their well-known effects on perception and mood, substances such as psilocybin (from so-called "magic mushrooms"), DMT (a component of ayahuasca), LSD and related ligands are showing consistent signals of immune modulation in laboratory and early clinical work. With inflammation underpinning many chronic illnesses—from rheumatoid arthritis and asthma to depression and cardiovascular disease—researchers are testing whether psychedelics, or drugs inspired by them, can safely dial down harmful immune responses without broadly suppressing immunity.
Scientific background: how psychedelics interact with immune pathways
Most classical psychedelics exert their central effects by activating the 5-HT2A receptor, a subtype of serotonin receptor that triggers intracellular signaling cascades in neurons. However, mounting evidence indicates these compounds also influence peripheral immune cells and brain-resident immune cells (microglia), modulating inflammatory signaling. In cell culture and animal models, specific psychedelics have been shown to reduce the release of pro-inflammatory cytokines—protein messengers such as TNF-alpha and IL-6—that drive tissue damage and sustain chronic inflammation.
Laboratory and animal evidence
In vitro experiments using human immune cells and in vivo animal studies report that DMT, LSD and the phenethylamine (R)-DOI can decrease cytokine production and blunt immune activation after inflammatory challenge. Notably, some preclinical models show that these anti-inflammatory effects can be achieved without the broad immunosuppression characteristic of glucocorticoid steroids, which leave patients vulnerable to infections and other complications. In an asthma model, two structurally related serotonergic compounds produced markedly different outcomes: (R)-DOI reversed airway inflammation entirely, while the analogue (R)-DOTFM had no effect—evidence suggesting that anti-inflammatory activity may be separable from hallucinogenic potency.
Human studies and emerging clinical signals
Early clinical work is consistent with mechanistic data. A randomized study of 60 healthy volunteers found that a single dose of psilocybin reduced blood concentrations of key inflammatory markers, including TNF-alpha and IL-6, for up to a week after dosing. Separately, clinical trials of ayahuasca (which contains DMT) in people with treatment-resistant depression observed decreases in C-reactive protein (CRP), an established marker of systemic inflammation; in those studies the magnitude of CRP reduction correlated with improvements in mood symptoms.
These findings reinforce a growing hypothesis in psychoneuroimmunology: inflammation contributes to certain mood disorders, and reducing inflammatory signaling may be one pathway by which psychedelic-assisted therapies deliver antidepressant effects. Nevertheless, human studies so far face limitations—small sample sizes, variable participant histories with psychedelic use, and the practical difficulty of blinding participants when subjective psychedelic effects make placebo control challenging. Expectation and context can influence mood and perhaps physiological endpoints, complicating interpretation.
Development of non‑hallucinogenic, psychedelic‑informed drugs
To harness the therapeutic immunomodulatory potential without eliciting hallucinations, researchers and companies are developing so-called "psychedelic-informed but psychedelic-inactive" molecules—sometimes abbreviated informally as "Pipi" drugs. These agents are designed to engage the same or related molecular targets that mediate therapeutic effects while avoiding the signaling events that produce altered perception. Examples in early development include DLX-001 and DLX-159 from Delix Therapeutics, which have demonstrated antidepressant-like signals in preclinical screens without inducing a full psychedelic subjective state. If anti-inflammatory benefits can be dissociated from hallucinogenic effects, these next-generation agents could offer new treatment classes for autoimmune and inflammatory disorders without the regulatory and logistical complexities of psychedelic-assisted psychotherapy.
Key implications and research priorities
The potential to introduce a novel anti-inflammatory mechanism has several implications: it could broaden therapeutic options for chronic inflammatory and neuroinflammatory diseases; reduce reliance on broad-spectrum immunosuppressants; and expand understanding of how neuromodulatory receptors influence peripheral immunity. Critical next steps for the field include larger, well-controlled clinical trials that enroll people with established inflammatory illnesses; improved placebo and masking strategies (for example, using active comparators that mimic some subjective effects without immunomodulatory action); and detailed molecular studies to map which intracellular pathways mediate immune outcomes.
Expert Insight
"The emerging data suggest psychedelics modulate immune signaling in ways we didn't anticipate ten years ago," says Dr. Elena Moreno, immunopharmacologist at the University of Cambridge. "If we can pinpoint receptor-level and downstream pathways responsible for anti-inflammatory effects, we can design therapies that retain clinical benefit without the psychoactive component. That would be a major advance for patients with chronic inflammatory diseases."
Regulatory and clinical challenges
Despite promising results, regulatory hurdles remain. Many psychedelics are scheduled substances in numerous jurisdictions, which complicates trial approval, manufacturing, and distribution. Ethical and clinical frameworks must also be developed for treatments that traditionally require therapeutic support during acute subjective effects. For non-hallucinogenic derivatives, regulators will demand robust safety and efficacy data before these agents can be positioned as standard anti-inflammatory medicines.
Future prospects
Integrating psychedelic pharmacology with immunology opens a path for translational discovery: from mechanistic cell studies to animal models, then to targeted clinical trials in conditions where inflammation is a causal factor. If ongoing and future studies confirm meaningful, reproducible reductions in cytokines and inflammatory biomarkers—and if those changes translate to durable clinical benefits—psychedelics or their derivatives could seed a new class of immune-modulating drugs. Research groups and biotech companies are already prioritizing this approach, coupling medicinal chemistry with modern immunophenotyping and biomarker-driven trial designs.
Conclusion
Psychedelic compounds are emerging as more than tools for psychopharmacology: they may reveal previously unrecognized levers for immune control. Early laboratory and human data show reductions in inflammatory mediators and correlations with symptom improvement in mood disorders. The crucial questions going forward are whether these effects are reproducible in larger, well-controlled clinical populations, whether anti-inflammatory mechanisms can be uncoupled from hallucinogenic action, and how best to translate these findings into safe, accessible therapies. The coming decade of research will determine whether the therapeutic promise of psychedelics extends beyond the mind to become a practical weapon against inflammation-driven disease.
Source: sciencealert


Leave a Comment