7 Minutes
Overview: When cooling systems become a health concern
Air conditioning (AC) improves comfort and reduces indoor humidity, but poorly maintained or malfunctioning systems can pose health risks. Microbiologists and indoor air-quality experts warn that contaminated HVAC systems can release allergens, chemical vapours and infectious microbes into enclosed spaces, contributing to so-called "sick building syndrome" and, in some cases, to outbreaks of respiratory and other infections. This article reviews the scientific evidence, identifies the main microbial and chemical hazards, and outlines practical prevention strategies for building managers and occupants.
What is sick building syndrome and how does it present?
Sick building syndrome (SBS) describes a collection of nonspecific symptoms experienced by people who spend prolonged time inside a particular building. Symptoms typically appear during occupancy and improve after leaving the environment. Common complaints include headaches, dizziness, nasal congestion or runny nose, persistent cough or wheeze, skin irritation or rashes, difficulty concentrating, and fatigue. SBS is most often reported by office workers and occupants of institutional settings such as hospitals or schools, but any enclosed workspace with poor indoor air quality can be affected.
Scientific context: SBS is not a single disease but a syndrome linked to indoor air quality, ventilation performance, humidity control and contaminant sources. Multiple factors—biological (mould, bacteria, viruses), chemical (volatile organic compounds from cleaning agents or refrigerant leaks) and physical (inadequate ventilation, dry air)—can interact to increase incidence.
Evidence from studies and clinical findings
Observational and cross-sectional studies have documented higher rates of SBS symptoms in air-conditioned workplaces compared with naturally ventilated environments. For example, a 2023 study in India compared 200 healthy adults who worked six to eight hours daily in air-conditioned offices with 200 adults who did not. The AC-exposed group reported more SBS symptoms over two years, showed a higher prevalence of allergic symptoms, had reduced lung function on clinical testing, and recorded more work absences than the non-AC group. Multiple independent studies have since corroborated increased SBS prevalence among AC office workers.
These findings do not mean air conditioning is intrinsically hazardous; rather, they highlight that poor maintenance, inadequate ventilation rates and contaminated components can convert an intended filtration and comfort system into a source of contaminants.

Microbial and chemical hazards linked to HVAC systems
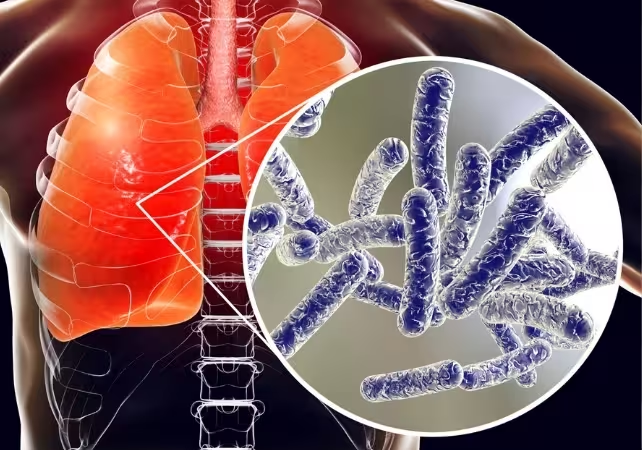
Legionella and water-borne bacterial pathogens
Legionella pneumophila, the bacterium behind Legionnaires' disease, thrives in warm, water-rich niches such as cooling towers, condensate pans and poorly maintained HVAC water systems. Legionnaires' disease is a severe pneumonia acquired by inhaling aerosolized water droplets containing the bacteria. Outbreaks commonly occur in communal settings (hotels, hospitals, office buildings) when building water systems are contaminated. Symptoms—cough, shortness of breath, chest pain, fever—appear two to 14 days post-exposure and often require hospitalization.
Fungi and moulds
Dust and moisture accumulation in ducts, drain pans and filters create habitats for fungi such as Aspergillus, Penicillium, Cladosporium and Rhizopus. In healthy people these spores can trigger allergic reactions and respiratory irritation. In immunocompromised patients, however, invasive fungal infections can become life-threatening, causing pneumonia, abscesses and dissemination to organs like the brain, liver and skin.
Viral transmission
While many viruses spread primarily via close contact or contaminated surfaces, there are documented instances where aerosols circulated by AC units contributed to airborne transmission. A reported case in a Chinese kindergarten implicated an AC unit in a restroom as the origin of an airborne norovirus outbreak affecting multiple children. Conversely, well-maintained systems with appropriate filtration and ventilation can reduce circulating levels of respiratory viruses, including SARS-CoV-2, by diluting indoor air and capturing viral particles.
How humidity, filtration and chemicals influence risk
Air conditioners lower indoor humidity, producing drier air than outdoors. Low relative humidity dries nasal and airway mucous membranes, weakening this first-line barrier against pathogens and increasing susceptibility to infections of the sinuses and lower airways. Filters, when clean and appropriately rated (MERV or HEPA where feasible), trap particulates, spores and some bacteria. However, dirty or clogged filters, neglected condensate pans and unclean coils can become reservoirs for microbes, releasing them back into the airflow.
Chemical exposures can also occur: vapours from cleaning agents, disinfectants, or refrigerant leaks may contain volatile organic compounds (VOCs) such as toluene, formaldehyde or other irritants that exacerbate respiratory symptoms and contribute to SBS.
Prevention, technologies, and best practices
Preventing AC-associated infections and minimizing SBS requires a combination of maintenance, monitoring and building design actions:
- Regular HVAC maintenance: scheduled inspection, cleaning and replacement of filters; cleaning of drain pans and coils; and preventative treatment of water systems.
- Appropriate filtration: use filters with suitable MERV ratings; consider HEPA filtration for high-risk areas (hospitals, immunocompromised wards).
- Humidity control: maintain indoor relative humidity in an optimal range (generally 40–60%) to limit mould growth and preserve mucosal defenses.
- Legionella control: implement water management programs, temperature control, and disinfection protocols for cooling towers and water systems.
- Ventilation and air exchange: increase outdoor air ventilation where possible to dilute indoor contaminants.
- Advanced technologies: ultraviolet germicidal irradiation (UV-C) inside ducts, bipolar ionization, and real-time air-quality sensors (IoT-enabled) can help reduce microbial loads and provide actionable data for building operators.
Key implications: proactive HVAC management reduces both nuisance symptoms of SBS and the risk of serious infections. Investing in maintenance, air-quality monitoring and occupant education delivers public-health benefits, lowers absenteeism, and improves productivity.
"Microbiologists and indoor air experts emphasize that air-conditioning systems are tools: when correctly designed, maintained and operated they improve health and comfort; when neglected, they can amplify contamination," say public-health specialists familiar with HVAC research.
Related research and future prospects
Ongoing research focuses on quantifying airborne pathogen dynamics in different HVAC configurations, the effectiveness of novel filtration and disinfection technologies, and smart building systems that integrate sensor networks with automated ventilation responses. Future advances in materials (self-cleaning surfaces), more efficient UV-C solutions, and robust building water management protocols promise to further reduce HVAC-associated risks.
Conclusion
Air conditioning itself is not inherently dangerous. However, improperly maintained or malfunctioning AC and HVAC systems can contribute to sick building syndrome and enable the spread of bacteria, fungi and—less commonly—viruses. Evidence from epidemiological studies and outbreak investigations highlights the importance of good ventilation design, regular maintenance, appropriate filtration, humidity control and water-system management. For building managers, facility engineers and public-health officials, prioritizing HVAC hygiene and monitoring is essential to protect occupant health and reduce the incidence of indoor air–related illness.
Source: theconversation

Leave a Comment