5 Minutes
The rhythmic hormonal fluctuations that define the menstrual cycle do more than regulate reproduction — they also produce measurable structural changes across the human brain. A longitudinal magnetic resonance imaging (MRI) study led by neuroscientists Elizabeth Rizor and Viktoriya Babenko at the University of California, Santa Barbara tracked 30 women through multiple cycle phases and documented coordinated alterations in white matter microstructure, cortical thickness, and cerebrospinal fluid volumes as hormone levels changed.
This research helps fill a longstanding gap: despite menstruation affecting roughly half the global population for decades of their lives, large-scale inquiry into how cycle-driven hormones reconfigure brain structure has been limited. The UCSB-led study provides one of the clearest human datasets showing that these effects extend beyond classical HPG-axis (hypothalamic-pituitary-gonadal axis) receptor-rich regions to influence brain-wide anatomy.
Scientific background and relevance
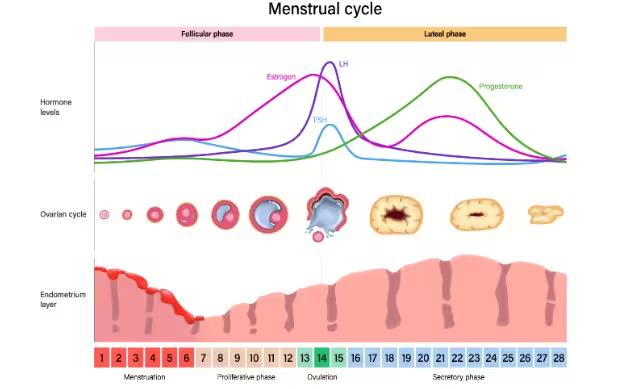
Hormones such as 17β-estradiol, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and progesterone rise and fall in predictable patterns across the menstrual cycle. Prior work has shown that hormonal transitions — like puberty, use of hormonal contraception, gender-affirming hormone therapy, and menopausal estrogen treatment — are associated with changes in white matter and cortical structure. White matter consists of myelinated axons that speed communication between gray matter regions; cortical thickness reflects the layered neurons and supporting tissue in the brain’s outer surface. Both are measurable with modern MRI techniques and are relevant to cognition and behavior.
Methods: imaging across three cycle phases
Study design
Researchers scanned each participant at three defined time points: menses, ovulation, and mid-luteal phase. At each visit they collected blood samples to quantify circulating hormone concentrations and used diffusion MRI and structural MRI sequences to assess white matter microstructure, cortical thickness, and cerebrospinal fluid (CSF) volume.
Key findings
The study reported coordinated, hormone-synchronous changes across the brain:
- Just before ovulation, when 17β-estradiol and luteinizing hormone levels surge, white matter microstructure exhibited signatures consistent with enhanced information transfer speed across brain networks. These changes suggest transient increases in the efficiency of neural communication tied to rising estradiol and LH.
- Increases in follicle-stimulating hormone (FSH), which helps mature ovarian follicles and peaks pre-ovulation, were associated with thicker cortical gray matter in multiple regions.
- After ovulation, during the mid-luteal phase when progesterone rises, researchers observed increased tissue volume alongside reduced cerebrospinal fluid volume in specific brain areas.
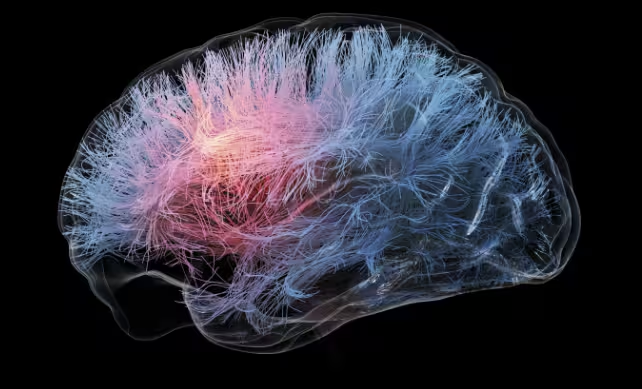
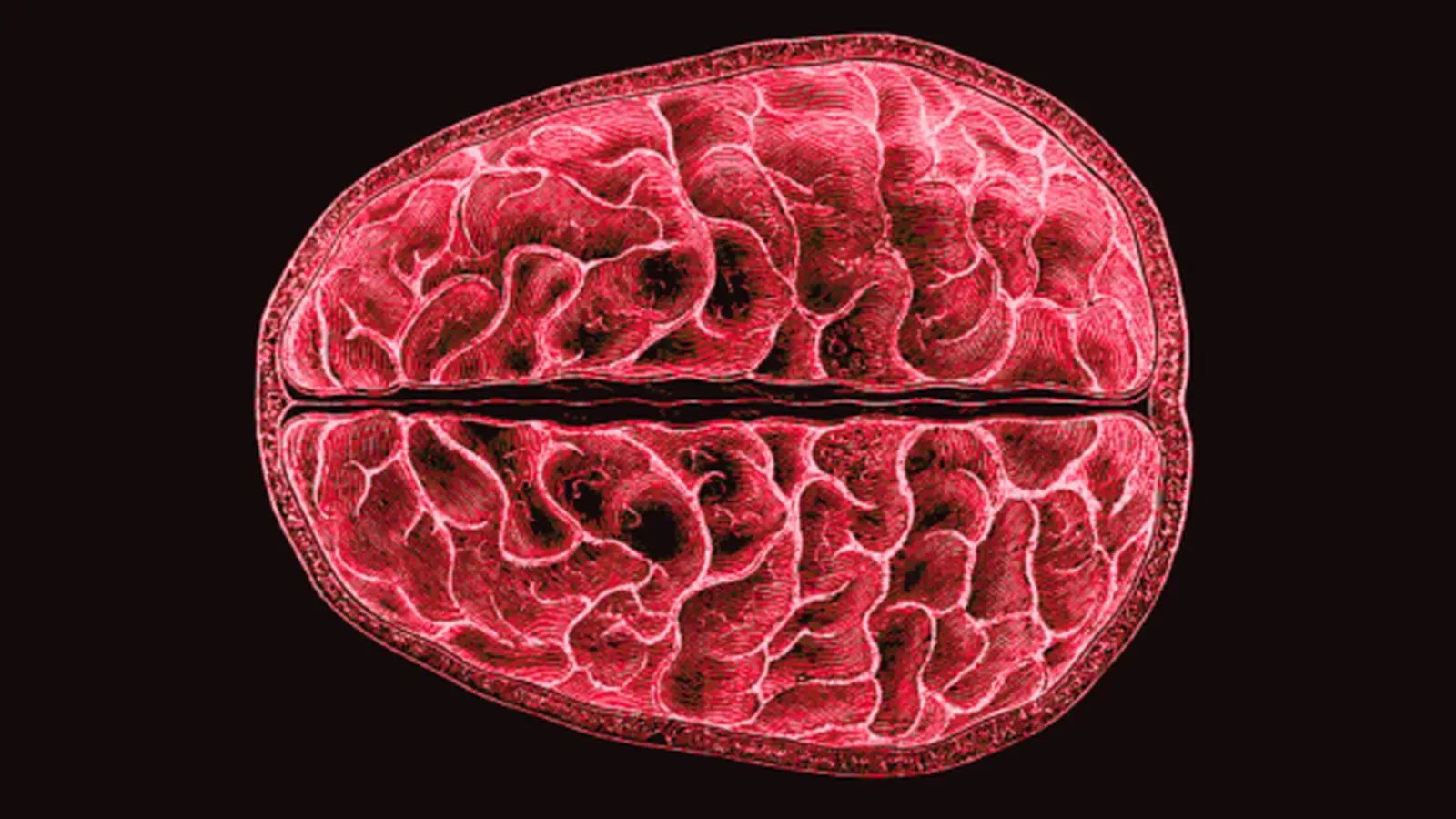
White matter tracts connecting regions in the human brain
The authors emphasize that these structural shifts occurred simultaneously across many brain regions, rather than being confined to classical hormone-receptive nuclei of the HPG axis.
Implications for cognition, mood, and clinical research
While the MRI measures document anatomical modulation by routine hormonal rhythms, the study does not directly link structural change to specific cognitive or behavioral outcomes. Nevertheless, the findings open several important avenues:
- Mechanistic studies can now test whether transient improvements in connectivity near ovulation correlate with measurable shifts in attention, memory, or processing speed.
- Understanding brain-hormone dynamics may clarify why a subset of individuals experience severe mood and cognitive disturbances tied to the menstrual cycle, such as premenstrual dysphoric disorder (PMDD).
- The results inform neuroimaging study design: investigators should consider menstrual phase as a potential confound or biological variable in studies involving women of reproductive age.
Future directions
Larger cohorts, repeated sampling across multiple cycles, and integration of functional MRI and behavioral testing will be needed to map cause–effect relationships between hormones, structure, and function. Multimodal imaging combined with hormonal challenge paradigms or hormone-suppression experiments could isolate which receptors and cellular processes drive the observed tissue dynamics.
Expert Insight
"The study underscores that the adult human brain is dynamically responsive to endogenous hormone rhythms, not static between menstrual cycles," says Dr. Claire Mendes, a fictional clinical neuroscientist specializing in neuroendocrinology. "This has practical implications: clinicians and researchers should account for cycle phase when assessing cognition or mood, and future trials should stratify or control for these biological fluctuations."
Conclusion
This longitudinal MRI work provides robust evidence that routine menstrual-cycle hormones drive brain-wide structural changes in white matter, cortical thickness, and CSF volume. Although the behavioral consequences remain to be determined, the findings establish an important baseline for future research into hormone-related cognition, mental health, and personalized medical approaches for people who menstruate.
White matter tracts connecting regions in the human brain. (Thom Leach/Science Photo Library)
Source: sciencealert

Leave a Comment