4 Minutes
A large retrospective analysis of nearly half a million medical records published in 2023 found repeated associations between serious viral infections and an elevated risk of neurodegenerative diseases, including Alzheimer's and Parkinson's. Researchers reported 22 reproducible links between prior viral exposure and later development of neurodegeneration after screening health records from multiple cohorts. The findings reinforce growing evidence that some viral illnesses and the inflammation they provoke in the nervous system may be important, potentially modifiable risk factors for dementia and related disorders.
Study design and key findings
The research team used an epidemiological, data-driven approach to scan medical records for connections between viral diagnoses and six major neurodegenerative diseases. The initial discovery phase compared roughly 35,000 Finnish patients diagnosed with neurodegeneration to 310,000 matched controls. That analysis produced 45 candidate associations, which the investigators then tested in an independent validation set from the UK Biobank—about 100,000 records—ultimately narrowing results to 22 robust links.

Notable findings included a dramatic association between viral encephalitis (inflammation of the brain caused by virus infection) and later Alzheimer's: patients with a history of viral encephalitis were found to have substantially higher odds of developing Alzheimer's disease. Severe respiratory infections such as pneumonia following influenza were associated with increased risks for Alzheimer's, dementia, Parkinson's disease and amyotrophic lateral sclerosis (ALS). Intestinal viral infections, viral meningitis and reactivation of varicella-zoster virus (the cause of shingles) also showed links to several neurodegenerative outcomes.
The study reported that some associations persisted for up to 15 years after the infection. Importantly, investigators did not observe any instances in which prior viral exposure reduced later neurodegenerative risk.
Biological context: neurotropic viruses and brain inflammation
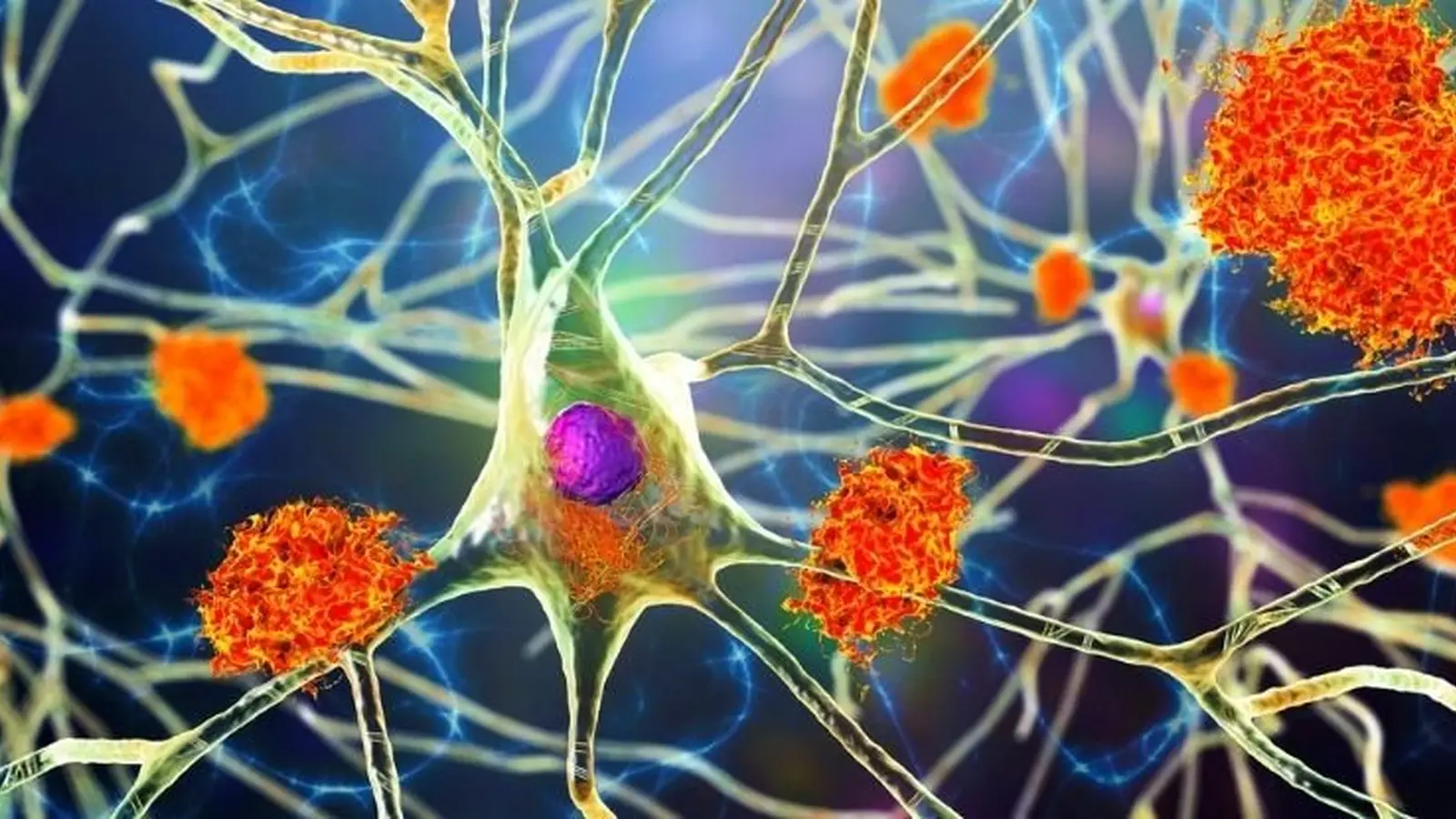
About 80% of the viruses implicated by the analysis are considered neurotropic—meaning they can cross or affect the blood-brain barrier and directly or indirectly trigger inflammation in neural tissue. Neuroinflammation is a recognized contributor to the pathophysiology of Alzheimer's, Parkinson's and other degenerative disorders. Viral infections may initiate or accelerate pathological processes such as protein misfolding, immune activation, or neuronal loss, although the observational design cannot establish direct causation.

Prior related evidence
These epidemiological signals build on other recent work: for example, a 2022 study linked Epstein–Barr virus infection with a markedly higher risk of multiple sclerosis. Together, such studies suggest a broader pattern in which common viral exposures can have long-term neurological consequences in susceptible individuals.
Public health implications and limitations
The authors emphasize that vaccines exist for several implicated pathogens—influenza, pneumococcal pneumonia and varicella-zoster—and that vaccination reduces hospitalization rates and severe disease. While vaccines do not eliminate all infections, reducing severe viral illness and the associated systemic and neural inflammation could plausibly lower downstream neurodegenerative risk at a population level.
However, the study is retrospective and observational: it can reveal associations but cannot prove that the viral infections caused the subsequent brain disease. Confounding factors, detection bias and differences in healthcare access or diagnostic coding may influence results. The investigators call for further mechanistic research and prospective studies to test causality and to explore whether targeted prevention (for example, vaccination or antiviral treatment) can alter long-term neurological outcomes.
Conclusion
This large-scale medical-record analysis adds to accumulating evidence that severe viral infections and the inflammation they provoke may increase the risk of neurodegenerative disorders. The results encourage further investigation into viral mechanisms of brain injury and strengthen the case for public-health measures—particularly vaccination—that reduce severe viral disease and hospitalizations.
Source: sciencealert

Leave a Comment