5 Minutes
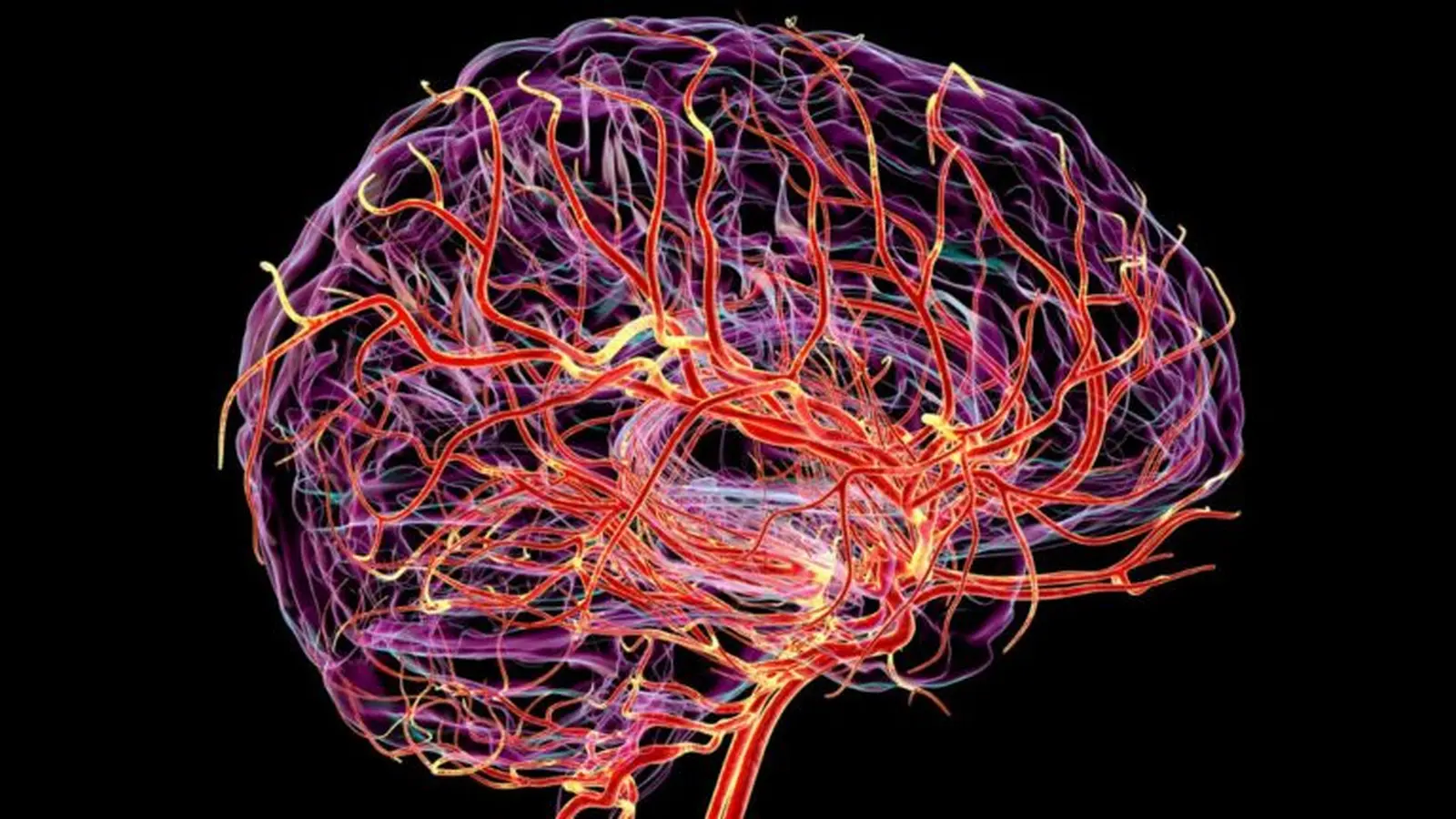
Researchers have developed a noninvasive MRI technique that maps tiny, rhythmic expansions and contractions of blood vessels across the living human brain. The approach could reveal how microvascular pulsations change with age and vascular risk factors—and whether those changes signal early dementia or cognitive decline.
A new window into the brain's microcirculation
Arterial pulsation acts like a subtle pump inside the skull, driving fluid movement and helping clear metabolic waste. Until now, detecting how microscopic arteries and capillaries pulse in people was difficult, limiting researchers to coarse measurements or animal models. A team at the University of Southern California, working with Siemens Healthcare US, combined two advanced MRI techniques to capture volumetric pulsatility across the entire cerebrovascular tree—from major branches down to the tiniest twigs.
How the imaging technique works
The new method merges vascular space occupancy (VASO) with arterial spin labeling (ASL). Briefly:
VASO: Measuring vessel volume
VASO detects subtle changes in the volume of blood vessels by measuring how blood displaces surrounding tissue signals. It’s sensitive to tiny expansions and contractions that occur with each heartbeat.
ASL: Tracking blood flow without contrast
ASL labels inflowing blood water as an endogenous tracer, allowing blood flow measurements without injected contrast agents. When combined with VASO, ASL helps distinguish flow-related effects from true volumetric pulsatility.
The hybrid approach gives researchers a first-of-its-kind, noninvasive view of dynamic microvascular behavior in living human brains.
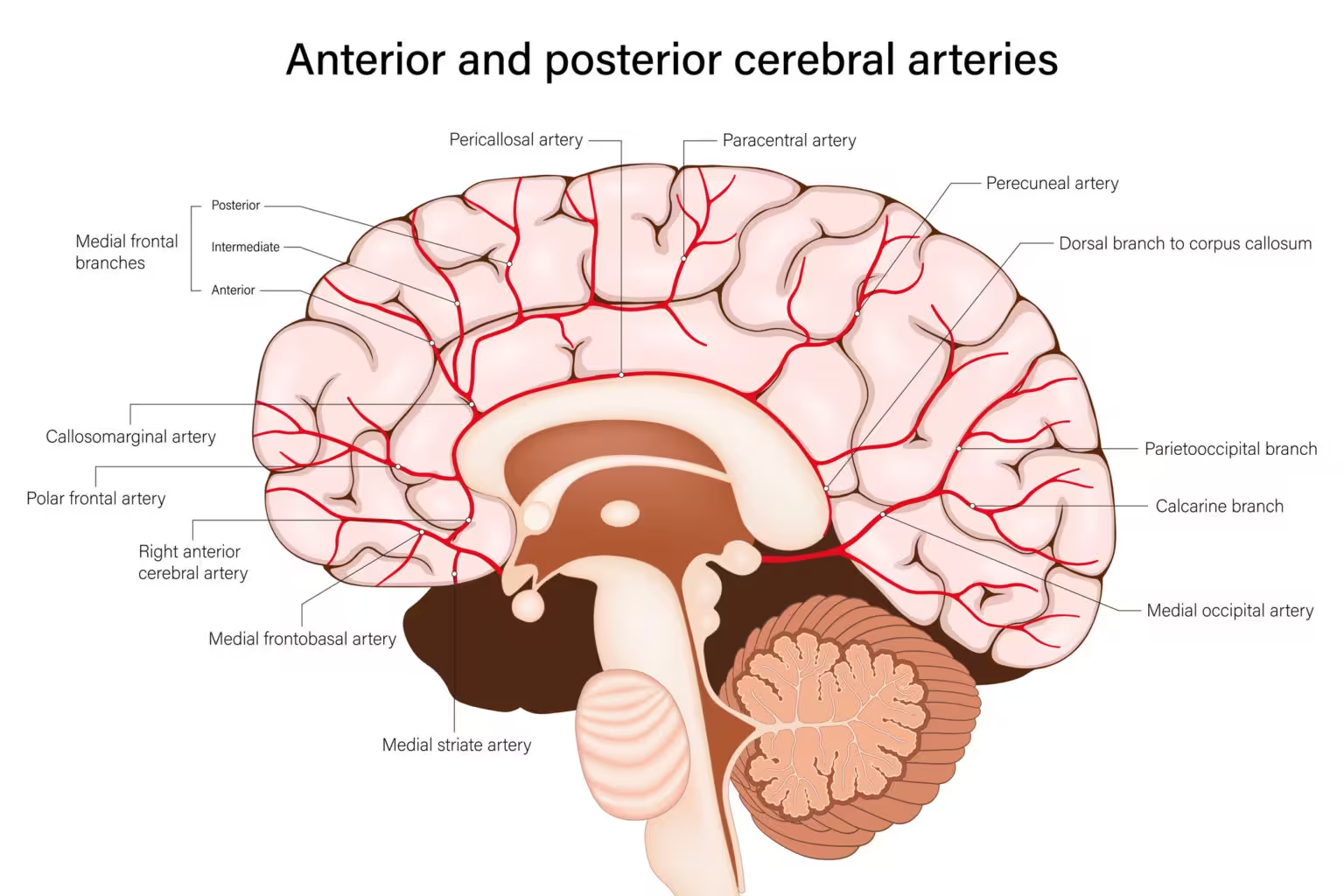
Cerebral arteries
What the study observed
Using the combined VASO–ASL protocol, the USC team scanned healthy volunteers across younger (20s–30s) and older (mid-50s–60s) age groups. They found that pulsatility increased in deep white matter with age, and the effect was more pronounced in older participants with hypertension. These human observations mirror recent animal work that linked increased white matter vascular pulsation to aging and small vessel disease.
Lead investigator Danny Wang describes arterial pulsation as a key mechanism for moving cerebrospinal fluid (CSF) and clearing waste from brain tissue. Coauthor Fanhua Guo adds that capturing volumetric pulsatility in both gray and white matter provides a missing bridge between large-vessel imaging and microscopic microvascular damage observed in dementia.
Why this matters for dementia research
Elevated arterial pulsation may reflect reduced microvascular density or branching with age—a structural decline that could make small vessels less able to absorb each pressure wave. If the remaining vessels amplify pulse volume to dissipate pressure, this altered dynamics could slow CSF movement and impair waste clearance, mechanisms implicated in Alzheimer’s disease and other dementias.
Importantly, prior associations between cerebrovascular pulsation and cognitive decline were largely inferred from animal studies or indirect human measures. This noninvasive MRI offers a direct way to test whether microvascular pulsatility predicts future cognitive impairment or serves as an early biomarker for small vessel disease.
Future prospects and clinical potential
The technique opens several avenues: longitudinal studies to track pulsatility changes over time, clinical trials to see if vascular risk reduction alters pulsation patterns, and integration with other imaging biomarkers such as amyloid PET or diffusion MRI. With further validation, volumetric pulsatility mapping could become a tool for early risk stratification, monitoring therapeutic response, or refining our understanding of how vascular health ties into neurodegeneration.
Expert Insight
"This imaging advance is exciting because it finally lets us see the microvascular choreography that likely underpins many aging-related brain changes," says Dr. Maya Patel, a fictional neurovascular researcher. "If elevated pulsatility precedes structural damage or cognitive decline, clinicians could intervene earlier—by treating hypertension, improving vascular resilience, or targeting CSF clearance pathways."
The USC study, published in Nature Cardiovascular Research, shows promise but also raises questions. Why do pulsations increase in white matter specifically? How do individual risk factors like hypertension, diabetes, or lifestyle interact with pulsatility? Answering these will require larger, diverse cohorts and longitudinal follow-up.
For now, the new VASO–ASL approach provides an important research tool: a scalable, noninvasive window into the brain’s smallest vessels, and a potential early indicator of vascular processes that may lead to dementia.
Source: sciencealert

Leave a Comment