4 Minutes
A novel gene therapy developed in London has put patients with a rare and aggressive form of leukemia into lasting remission. The experimental treatment, known as BE-CAR7, converts donor T cells into ready-to-use cancer fighters using precision genetic edits. Early results from trials at Great Ormond Street Hospital and King's College London show deep remissions and new hope for children and adults who previously had few options.
Why T-cell acute lymphoblastic leukemia is so hard to treat
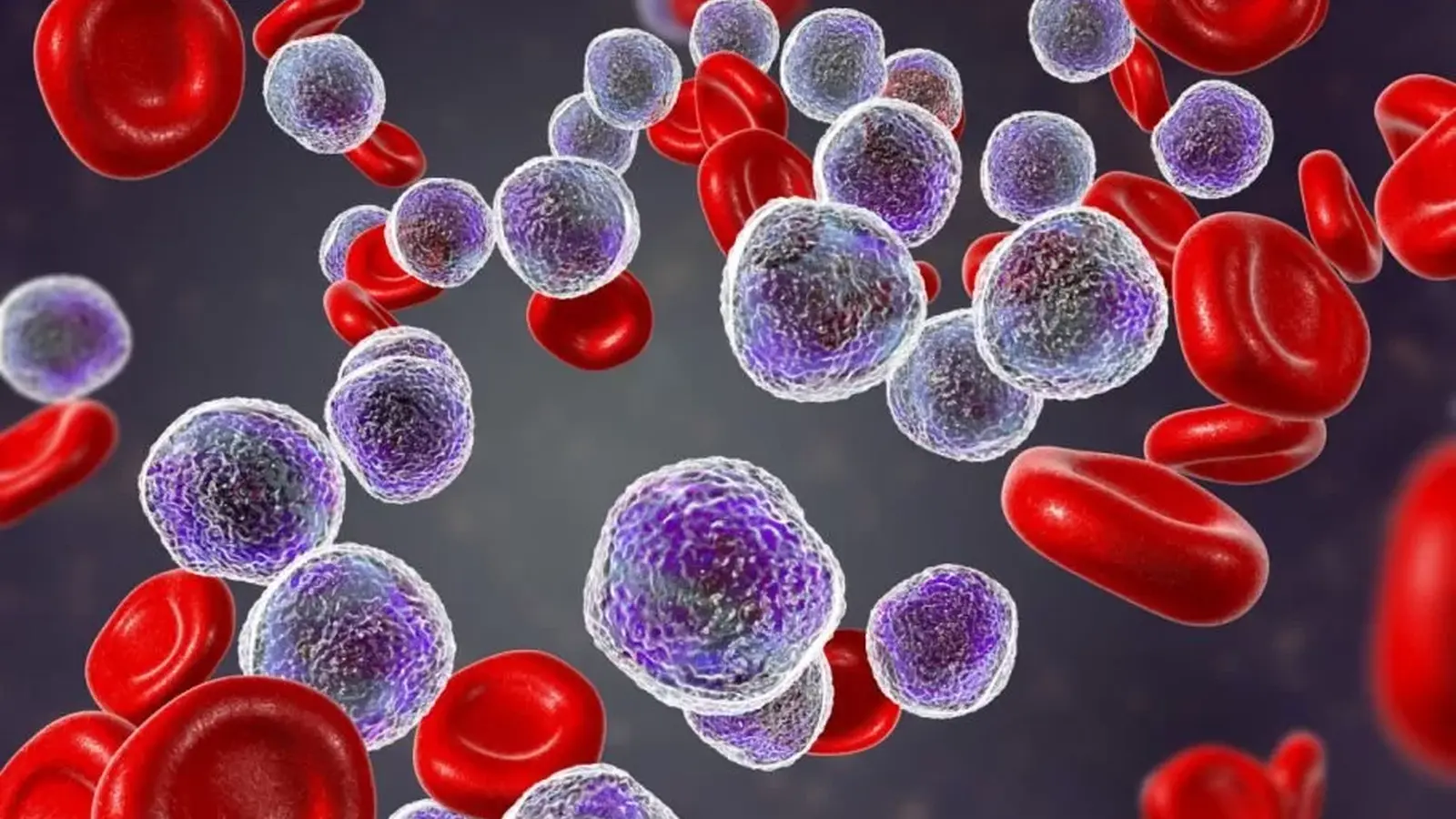
T-cell acute lymphoblastic leukemia (T-ALL) arises when T cells — a frontline component of the immune system — begin to grow uncontrollably. Unlike more common B-cell leukemias, T-ALL is biologically distinct and, in a minority of patients, resists standard chemotherapy. That treatment gap has driven researchers to explore advanced cellular therapies such as CAR T cells and precision gene editing.
How BE-CAR7 turns donor cells into off-the-shelf cancer killers
The BE-CAR7 approach starts with T cells taken from a healthy donor. Researchers apply three separate, targeted genetic edits to those donor T cells so they can safely attack the patient's cancer without needing a precise tissue match. The technology—described by the team as an ultra-precise editor—changes single genetic letters to reprogram cell behavior. The result is an allogeneic (donor-derived) CAR T product that can be given immediately, rather than custom-made for each patient.

Designed for short-term dominance, then replacement
BE-CAR7 cells are engineered not only to kill malignant T cells but also to be cleared from the patient within a controlled window. If the edited donor cells disappear within roughly four weeks, clinicians can then perform a bone marrow transplant to rebuild a healthy immune system. This two-step strategy—rapid tumor control followed by curative transplantation—aims to reduce relapse while managing long-term safety.
Early trial outcomes and patient stories
The published trial included ten patients: eight children and two adults with refractory or high-risk T-ALL. About 82% entered a state the investigators call a very deep remission and were able to proceed to stem cell transplantation. Overall, 64% of participants remained disease-free at the reported follow-up, with roughly two-thirds still without signs of relapse up to three years after treatment.
One of the first recipients was 16-year-old Alyssa Tapley, who received the therapy about three years ago for an aggressive T-ALL and is reported to be living disease-free. Those individual successes underscore the potential real-world impact of this method.
Great Ormond Street Hospital’s charity has committed to funding treatment for 10 more patients while the team refines dosing and follow-up protocols. The full trial report was published in the New England Journal of Medicine, providing peer-reviewed detail on safety and efficacy.
What this means for future cancer care
Dr. Rob Chiesa, a transplant specialist involved in the study, noted: "Although most children with T-cell leukemia respond well to conventional treatments, about 20% do not. This group urgently needs better options, and these results offer fresh hope for the future."
BE-CAR7 exemplifies two converging trends in oncology: off-the-shelf, allogeneic cellular therapies and high-precision gene editing. If larger trials confirm these early results, the approach could scale more readily than bespoke CAR T products and offer rapid treatment for aggressive blood cancers.
Next steps and open questions
Important questions remain: how durable are remissions beyond three years, what late toxicities could appear, and how broadly applicable is this method across patient ages and disease subtypes? Regulators and clinicians will watch closely as the team expands enrollment and follows patients longer. For families and physicians facing refractory T-ALL, BE-CAR7 represents a promising, science-driven option that may reshape the standard of care.

Leave a Comment