6 Minutes
Record-breaking birth and why it matters
A newborn in the United States has captured global attention after being born from an embryo that had been cryopreserved for more than 30 years. The embryo was created and placed into long-term storage in 1994, an era when the internet and mobile phones were nascent technologies. The case sets a new benchmark for long-term embryo viability and raises scientific, legal, and ethical questions about assisted reproductive technology (ART), embryo donation, and how people connect with their genetic origins across decades.
Scientific background: IVF, cryopreservation and embryo storage
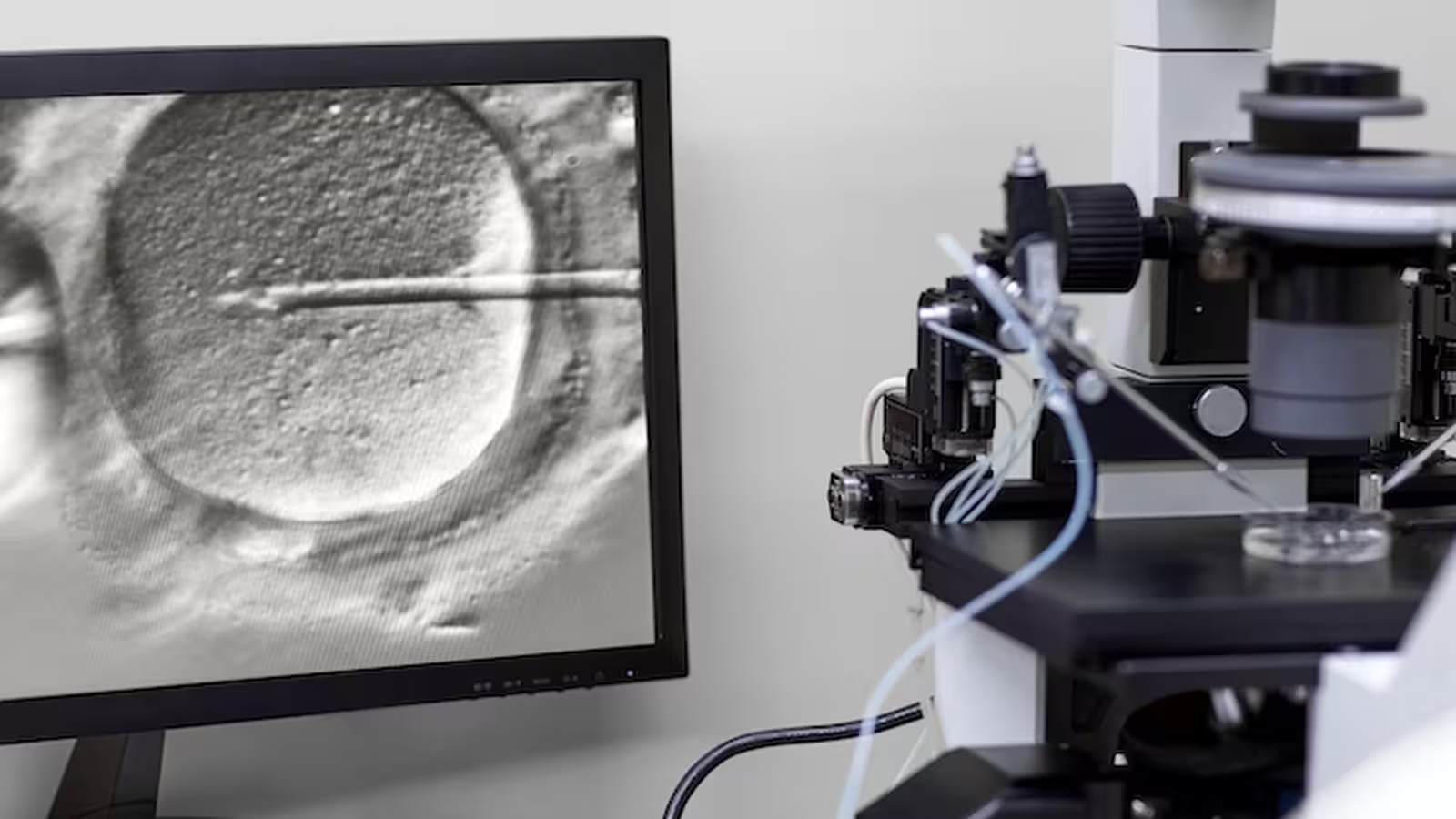
In vitro fertilisation (IVF) routinely produces multiple embryos during a treatment cycle. Advances in cryopreservation, particularly vitrification, have dramatically improved freezing outcomes by preventing ice crystals that can damage cells. Embryo freezing is now an established component of IVF and fertility preservation. Cryopreservation extends the window for pregnancy attempts and enables embryo donation, preimplantation genetic testing, and fertility planning for later life.
How embryos are preserved
Cryopreservation stabilises cells at very low temperatures, typically in liquid nitrogen at about -196°C. Modern vitrification techniques cool embryos rapidly to avoid crystal formation, increasing survival rates after thawing. Although short-term results have been well-documented, long-term storage introduces practical questions about viability, storage integrity, and policy: how long can embryos remain cryopreserved while still producing healthy live births?
The case, donation pathways and legal frameworks
Unlike many clinic-handled donations, the embryos in this case were transferred via a US nonprofit organisation that facilitates directed embryo donation, allowing donors to select recipients. The original donor, now in her 60s, chose this route in part because any child derived from those embryos would be a full genetic sibling to her adult daughter. That potential sibling relationship — with a generational gap exceeding three decades — highlights a novel family dynamic made possible by prolonged embryo storage.
Legal frameworks for embryo storage vary internationally. The United States has no federal statutory limit on how long embryos can be stored; storage duration is typically governed by clinic policy or state law. In contrast, the United Kingdom recently extended its statutory maximum storage period to 55 years, signaling a regulatory willingness to accommodate very long-term cryostorage. These divergent regimes mean that cross-border fertility care can create complex legal and ethical situations when embryos move between jurisdictions.
Social and psychological implications: identity, kinship and age gaps
Births from decades-old embryos create an unusual temporal disjunction: conception in one era, birth in another. This raises questions about identity and narrative for donor-conceived individuals. Research on donor-conceived families generally reports good family functioning, but the experience of being 'frozen in time' is distinct. People born from long-stored embryos may face questions about their place in family histories, the age of genetic relatives, and how to interpret relationships with donors or half-siblings who may be decades older or deceased.
Direct-to-consumer genetic testing platforms such as 23andMe and Ancestry.com have already transformed how donor-conceived people locate biological relatives. As prolonged embryo storage becomes more common, consumer DNA databases will likely be used increasingly to connect across generational gaps, sometimes circumventing regulated registries. That trend has implications for privacy, the expectations of donors and recipient families, and the social dynamics of forming relationships across large age differences.
Ethical and policy considerations
Long-term embryo storage surfaces ethical dilemmas that combine bioethics, reproductive autonomy, and family rights. Common questions include: What should clinics communicate to donors about long-term storage costs and eventual disposition? How should consent be structured to allow donors agency, while protecting future children's rights to information? What are the responsibilities of regulators in setting maximum storage periods and cross-border safeguards?
A reproductive medicine specialist commented that 'the science of cryopreservation has outpaced some of our social and legal frameworks. We need clearer guidance on consent, storage limits, and how to support donor-conceived people seeking information about genetic relatives.' Such guidance would need to balance donor autonomy, recipients' needs, and the welfare and privacy of those conceived from long-stored embryos.
Related technologies and future prospects
Beyond vitrification, improvements in embryo culture, genetic screening, and storage logistics will likely increase both success rates and the number of embryos in long-term cryostorage. Globalisation of fertility services — including international transport of gametes and embryos — amplifies the need for harmonised standards to manage donor numbers, prevent inadvertent consanguinity risks, and protect cross-border privacy expectations.
In parallel, as consumer DNA testing expands and medical records digitise, future-born individuals may have unprecedented access to genetic and contextual information about donors and genetic relatives. This could aid identity formation but also pose novel psychosocial challenges when familial ties span multiple decades.
Conclusion
The birth from a 30-year-frozen embryo underscores both the technical robustness of modern cryopreservation and the complex human questions it raises. Scientifically, this case demonstrates that embryos frozen for decades can still result in healthy live births, reinforcing the efficacy of vitrification and long-term storage protocols. Socially and ethically, it compels fertility clinics, regulators, and families to confront issues of consent, donor selection, cross-border regulation, and how donor-conceived individuals understand their origins when genetic relatives belong to a different era.
As assisted reproductive technologies continue to evolve, policymakers and clinicians will need to update guidelines on storage duration, donor information access, and support services for donor-conceived people. The interplay between reproductive medicine, consumer genetics, and family narratives will shape how society navigates these unprecedented temporal connections in the years ahead.
Source: theconversation

Leave a Comment