5 Minutes
New research suggests that not all depressive symptoms are equal when it comes to dementia risk. A long-term UK study finds six specific midlife symptoms that are linked to higher rates of dementia decades later — and those signals could help clinicians target early prevention.
Which depressive signs matter most?
The study, led by researchers at University College London, tracked 5,811 people over roughly 20 years. Researchers collected mental-health data between 1997 and 1999 when participants were 45–69 and dementia-free, then followed health records through 2023. Overall, 10.1% of participants eventually received a dementia diagnosis.
Rather than implicating depression as a single, uniform condition, the team identified six individual symptoms that accounted for the increased risk. These were:
- Losing self-confidence
- Difficulty coping with problems
- Not feeling affection for others
- Persistent nervousness
- Difficulty concentrating
- Dissatisfaction with how tasks are carried out
People who reported five or more depressive symptoms in midlife had a 27% higher dementia risk overall. But that elevated risk was largely driven by the six symptoms above. Two stood out: loss of self-confidence and trouble coping with problems were each associated with about a 50% higher dementia risk on their own.
The authors point out that other depressive features — such as sleep disturbances or suicidal thoughts — showed no clear long-term link with dementia in this cohort.
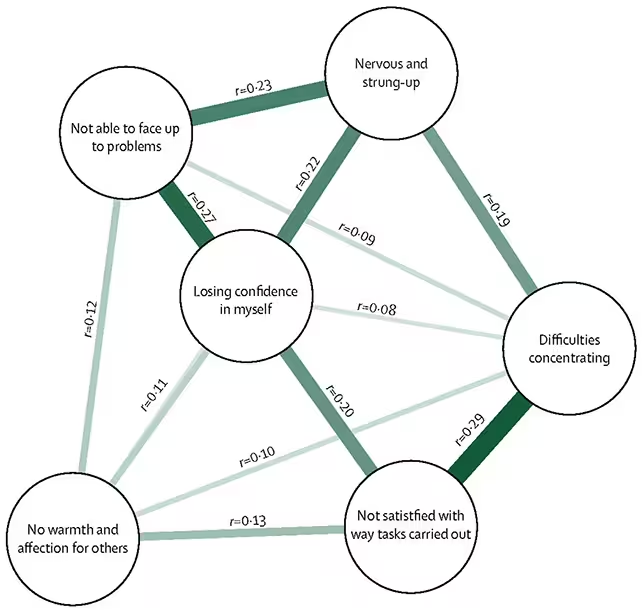
The researchers linked six symptoms of depression with dementia risk
How the study was done and what the numbers mean
This was a longitudinal observational study: an efficient way to find patterns over decades, but one that cannot prove cause and effect. Health outcomes were obtained from national registries and medical records, and mental-health measures were taken at baseline using established symptom inventories.
Why does this matter? If certain emotional or cognitive patterns in midlife reliably mark later vulnerability, clinicians could flag higher-risk people earlier and test prevention strategies — from lifestyle changes to more targeted mental-health care.
Biological and behavioral links worth watching
Depression and dementia share several plausible pathways. Chronic stress and depression can worsen cardiovascular health, increase inflammation, and reduce cognitive reserve — all factors that contribute to many forms of dementia. Symptoms such as poor concentration or persistent anxiety may reflect early brain changes, or they might accelerate decline by changing sleep, activity, or social engagement.
Understanding which symptoms carry the most prognostic weight helps refine models of risk. It also moves the conversation away from treating “depression” as a single risk marker and toward a more nuanced, symptom-level perspective.
Limits of the findings: who was studied?
The UCL team notes important caveats. Participants came from a long-running UK cohort made up largely of civil servants — a group generally healthier than national averages. Dementia rates in the study were lower than in wider UK populations, so the exact risk numbers may not generalize globally. More research is needed in diverse populations and across different healthcare systems.
Still, the signal is clear: certain midlife emotional and cognitive complaints appear to contain useful information about later brain health.
What this could mean for prevention
Targeted screening in primary care could pick up the specific symptoms flagged by the study. From there, clinicians might offer interventions known to support brain health: treating cardiovascular risk factors, promoting exercise and social engagement, addressing chronic stress, and providing tailored psychological therapies.
Crucially, the symptom-level approach could also inform research into biological mechanisms — helping scientists ask whether these midlife signs reflect early neurobiology, social factors that shape cognitive reserve, or some combination of both.
Expert Insight
"When we speak about dementia prevention, timing is everything," says Dr. Elena Morales, a neurologist specializing in cognitive disorders. "Midlife is a window where small adjustments — treating high blood pressure, improving sleep, or addressing persistent anxiety — can shift long-term trajectories. Studies that identify which symptoms are most predictive give clinicians practical signals to act on sooner."
Research like this doesn’t offer deterministic predictions for individuals, but it does open pathways for earlier, more personalized prevention strategies. As populations age worldwide, those incremental gains could translate into meaningful reductions in dementia cases.
Future studies must replicate the findings in broader samples and test whether intervening on the highlighted symptoms actually changes outcomes. For now, the take-home is simple: some everyday midlife struggles may tell us more about later brain health than we realized — and paying attention could matter.
Source: sciencealert
Comments
mechbyte
Is this even true? sample was civil servants, lower dementia rates so maybe not generalisable. need more diverse studies
bioNix
Wow didnt expect loss of self-confidence to predict dementia so strongly... kinda scary, makes me rethink midlife checkups


Leave a Comment