8 Minutes
Invisible to our ears but powerful in the clinic, focused ultrasound is emerging as a noninvasive way to treat brain disorders and cancer. Recent advances let clinicians aim concentrated sound energy at tiny tissue volumes to open barriers, deliver drugs, stimulate immune responses and, in some cases, destroy diseased tissue — all without scalpels or radiation.
How focused ultrasound harnesses inaudible sound
Ultrasound uses sound waves above the range humans can hear to create medical images and, increasingly, to treat disease. A transducer converts electrical signals into mechanical vibrations; those waves travel through the body, bounce off tissue boundaries and return as echoes that computers reconstruct into images. But when those same waves are focused into a small target — often a volume no larger than a grain of rice — their mechanical and thermal effects change. Focused ultrasound can heat tissue, push on vessel walls, or cause tiny gas bubbles suspended in the bloodstream to oscillate. Those effects make a range of therapeutic strategies possible.
MRI-guided focused ultrasound systems add a second layer of control. Imaging lets clinicians visualize the target in real time, monitor temperature changes and steer dozens to thousands of tiny sound beams so they converge precisely where needed. Early experiments more than 80 years ago showed that concentrated ultrasound could ablate brain tissue — similar to focusing sunlight with a magnifying glass — but it took decades of improvements in imaging, transducer arrays and acoustic modeling before clinicians could reliably and safely use focused ultrasound in the brain.
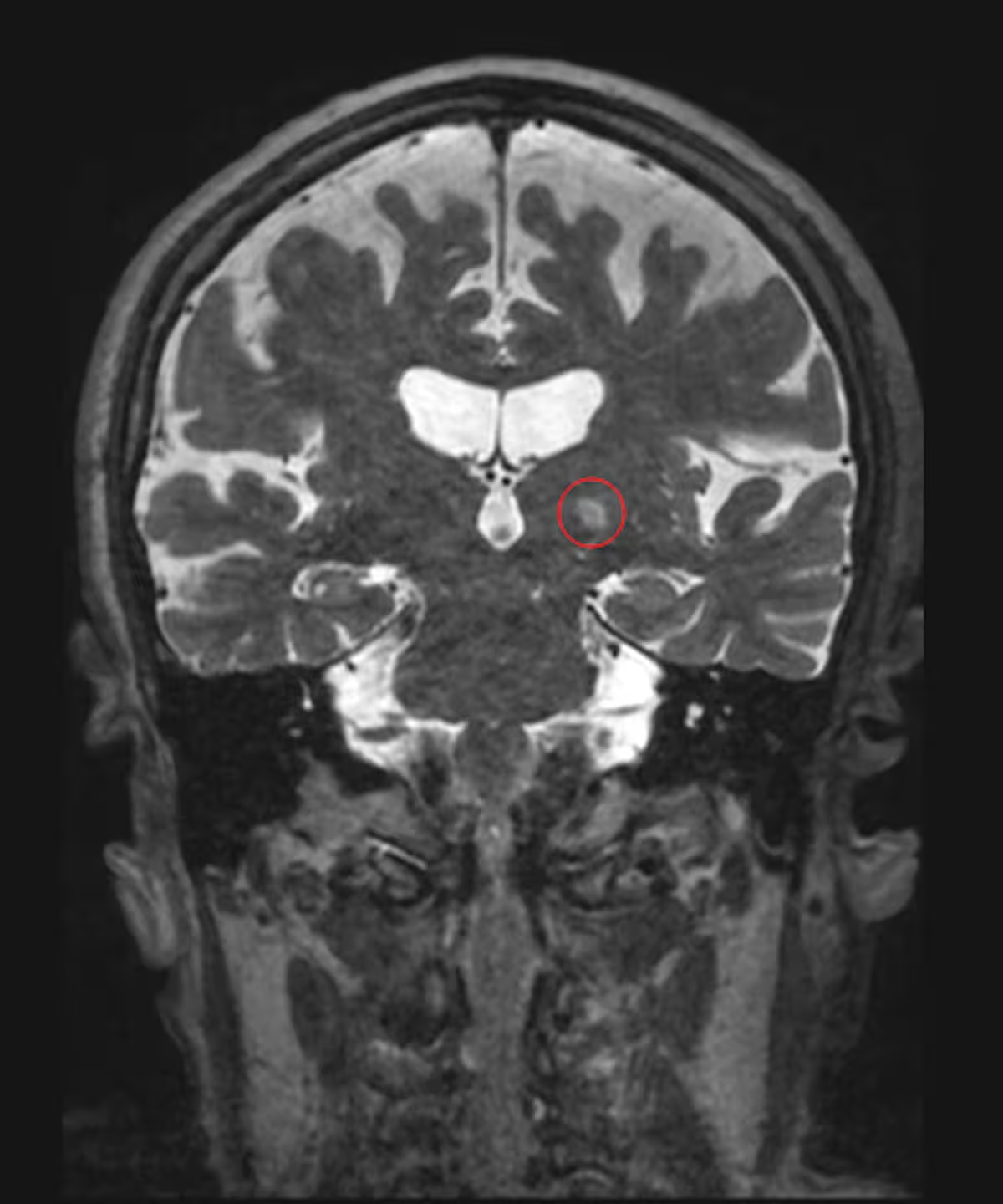
MRI of a patient treated for essential tremor using focused ultrasound, with the targeted part of the brain circled in red. (Jmarchn/Wikimedia Commons, CC BY-SA)
Opening the blood-brain barrier — a targeted door for medicines
The blood-brain barrier (BBB) is a tightly regulated cellular shield that protects the brain by limiting what can pass from circulation into neural tissue. That protection also blocks many drugs, large molecules and gene therapies from reaching diseased regions. Focused ultrasound offers a selective solution: low-intensity pulses aimed at a defined spot cause microbubbles already present in the blood to vibrate. The microbubbles’ oscillation temporarily loosens the tight junctions of the blood vessel wall, creating nanoscale pores that allow therapeutic agents to slip into the brain — but only where the ultrasound is applied.
This targeted BBB opening has been validated in animal studies and early human trials. Researchers have tested focused ultrasound to boost chemotherapy delivery to glioblastoma and brain metastases, and to increase the concentration of experimental Alzheimer’s therapies in affected brain regions. Parallel studies show promise for delivering viral vectors and other gene therapy vehicles that normally can’t cross the BBB, making genetic treatments for neurodegenerative and developmental brain diseases a more realistic goal.
Why this matters
- Precision: Only the ultrasound-targeted zone becomes permeable, reducing systemic side effects.
- Repeatability: The procedure can be performed multiple times, enabling staged dosing or booster treatments.
- Compatibility: Focused ultrasound can augment existing drugs and therapies rather than replace them.
Wakening the immune system: ultrasound plus immunotherapy
Many solid tumors are immunologically “cold”: they fail to attract immune cells or present few recognizable signals to trigger an attack. Focused ultrasound can change that. By mechanically disrupting a tumor or heating it in controlled ways, ultrasound breaks tumor cells into fragments and releases tumor antigens. These fragments can travel to lymph nodes where immune cells learn to recognize and target the cancer.
Laboratories and early clinical programs are exploring combinations of focused ultrasound with checkpoint inhibitors and other immunotherapies. The goal is to turn cold tumors — such as some pancreatic, breast and brain cancers — into hot ones that respond to systemic immune-based drugs. In 2022, the University of Virginia opened a dedicated center to accelerate immuno‑oncology research using focused ultrasound, and investigational trials have begun combining ultrasound with immunotherapies for advanced melanoma and other cancers.
Examples in practice
- Direct ablation: High-intensity focused ultrasound (HIFU) can thermally destroy small tumors without an incision.
- Immune priming: Sub-ablative ultrasound can release tumor antigens and inflammatory signals to enhance immune recognition.
- Drug delivery: Ultrasound-mediated vascular opening improves local delivery of chemotherapies or antibody drugs.
Beyond common diseases: rare disorders and structural lesions
While cancer and Alzheimer’s draw much of the spotlight, focused ultrasound also has potential for rare vascular and structural brain disorders. One example is cerebral cavernous malformation (CCM), a condition in which abnormally proliferating blood-vessel cells form fragile lesions that can bleed or cause seizures. Surgery is often the standard of care, but some lesions are deep or adjacent to critical tissue, making surgery high risk.
Preclinical work suggests that focused ultrasound can both improve drug delivery to CCMs and — surprisingly — stabilize lesion growth in animal models even without concurrent medication. The mechanism remains under study, but the observation has motivated neurosurgeons to plan early-phase clinical trials. If replicated in people, focused ultrasound could offer a less invasive option for managing some CCMs and other hard-to-reach brain lesions.
Technical hurdles, safety and the path to wider adoption
Focused ultrasound is not a one-size-fits-all remedy. The skull’s shape and density can distort sound waves, requiring individualized acoustic models and large multi‑element transducer arrays to compensate. Temperature monitoring and real-time imaging are essential to ensure patient safety and to avoid unintended injury. Moreover, regulatory approval depends on disease-specific trials that demonstrate not only safety but meaningful clinical benefit compared with existing standards of care.
Despite these challenges, hundreds of clinical trials have launched worldwide testing focused ultrasound for a variety of neurological and oncological applications. Essential tremor is already treated routinely with ultrasound in many centers, and ongoing trials target glioblastoma, metastatic brain disease, Alzheimer’s, and multiple rare CNS conditions.
Future directions: combining technologies for smarter therapies
The most exciting prospects come from pairing focused ultrasound with emerging modalities: targeted nanoparticles, gene-editing vectors, and advanced immunotherapies. Imagine delivering CRISPR tools just to a tumor or affected brain region, or using ultrasound to steer nanoparticle payloads that release drugs only after the BBB is opened. These hybrid approaches promise to raise efficacy while limiting systemic toxicity.
Engineers are also miniaturizing ultrasound systems and improving beam steering, which may enable ambulatory or outpatient treatments and expand access beyond specialized centers. As acoustic modeling, imaging and real-time feedback systems mature, clinicians will gain tighter control over where and how ultrasound acts at cellular and molecular scales.
Expert Insight
"Focused ultrasound is a toolbox, not a single therapy," says Dr. Elena Morales, a biomedical engineer who collaborates with clinical teams on device development. "Its strengths are precision and flexibility — you can tune the energy to open the blood-brain barrier, heat tissue just enough to kill tumor cells, or create mechanical forces that alert the immune system. The challenge now is integrating it intelligently with drugs and biologics to solve real clinical problems."
Her assessment echoes a wider sentiment in translational research: focused ultrasound's greatest value may be as an enabling technology that makes other therapies work better.
What patients and clinicians should know now
For patients exploring focused ultrasound, it's important to ask whether a treatment is part of an approved protocol or a clinical trial, what the known risks are for the specific procedure, and how the team will monitor and follow up. For clinicians, integrating focused ultrasound into practice requires collaboration across specialties — neurosurgery, radiology, oncology, engineering and immunology — to design trials that clearly measure clinical benefit.
Focused ultrasound has moved rapidly from an experimental physics curiosity to a clinically relevant technology. The next decade will test whether its promise — targeted drug and gene delivery, immune activation against tumors, and safer treatment options for rare brain diseases — translates into durable outcomes for patients.
Source: sciencealert
Comments
Armin
Is this even true? opening the BBB sounds risky, repeated sessions, immune stuff, long term effects? need solid trials before hype
mechbyte
wow didnt expect ultrasound to do so much, feels like magic tech. If they sort safety and costs, huge win. curious about side effects tho


Leave a Comment