5 Minutes
As dementia diagnoses climb with an ageing global population, a growing body of research suggests that a surprising share of those cases may have a different origin: the liver. New analyses indicate that up to 13% of people labeled with dementia in the United States could instead be experiencing cognitive decline caused by liver dysfunction — a condition that, in many cases, is at least partially reversible.
How liver disease can mimic dementia
Hepatic encephalopathy (HE) is the medical term for cognitive impairment that results from liver failure or severe liver dysfunction. When the liver can’t adequately filter toxins and regulate body chemistry, those imbalances affect many organs — notably the brain. Symptoms can include memory lapses, confusion, difficulty concentrating, motor problems such as tremors or falls, and even hallucinations. To clinicians seeing these signs in older patients, the picture can look remarkably like primary neurodegenerative dementia.
HE is common in advanced liver disease: more than 40% of people with cirrhosis develop some degree of encephalopathy. Yet the link between liver health and cognition often goes unrecognized in dementia clinics. As hepatologist Jasmohan Bajaj noted in 2024, health care providers must be aware of the overlap between dementia syndromes and treatable hepatic encephalopathy.
The data behind the misdiagnosis concern
Researchers led by teams at Virginia Commonwealth University reviewed large medical record databases to test how often liver disease markers appear in people recorded as having dementia. In an initial study of 177,422 US veterans diagnosed with dementia between 2009 and 2019, investigators found that more than 10% had high FIB-4 scores — a routinely used index that estimates liver fibrosis (scarring) from standard blood tests — even though none had a formal liver-disease diagnosis on file.
To see whether that finding applied beyond a veteran population, the team repeated the analysis in a broader national sample of 68,807 patients. The result was striking: almost 13% of those diagnosed with dementia had elevated FIB-4 scores, suggesting they were likely to have significant liver scarring or cirrhosis.

Up to 13 percent of people diagnosed with dementia in the US may have a misdiagnosis. (Rido/Canva)
Why this matters: treatment and reversibility
The key implication is clinical: hepatic encephalopathy is often treatable or manageable, particularly when identified early. Interventions range from dietary changes and medication to reduce blood ammonia and other toxins, to addressing the underlying liver disease drivers — such as viral hepatitis, alcohol-related injury, obesity-related nonalcoholic fatty liver disease, diabetes, and high cholesterol.
Case reports and clinical experience show dramatic improvements. In at least two patients previously labeled with dementia, treating hepatic encephalopathy resolved memory loss, tremors, falls, and hallucinations — restoring personality and function to the delight of their families. "He is a different person," one spouse observed after treatment reversed symptoms that had been written off as progressive dementia.
Cirrhosis — the replacement of healthy liver tissue with scar tissue due to persistent damage — magnifies these risks because it compromises detoxification and metabolic regulation. Yet recent animal studies suggest that some age-related liver changes might be reversible if interventions begin early, offering hope that cognitive benefits could follow improved hepatic health.
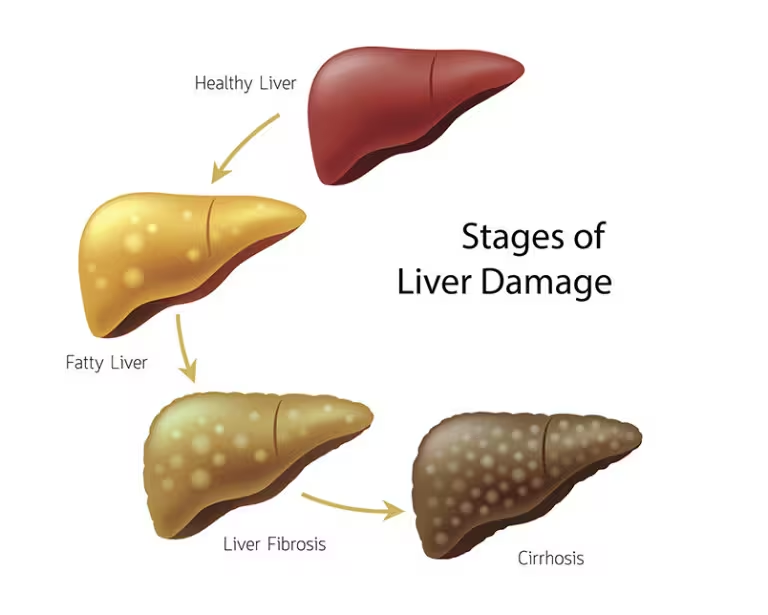
Cirrhosis is the result of persistent liver damage, where healthy tissue has been gradually replaced with scar tissue. (Kuo Du et al., Nature Aging, 2024)
Health disparities and missed opportunities
The researchers also found demographic patterns among patients with high FIB-4 scores. A greater proportion were non-white, hinting at health disparities in access to care for both liver disease and dementia diagnostics. The authors note that barriers to early screening and treatment — from limited specialty access to socioeconomic obstacles — could help explain unequal burdens of undetected liver-related cognitive impairment.
Because liver dysfunction affects multiple organs — kidneys, pancreas, heart, and brain — screening for liver disease in patients with new or atypical cognitive complaints is a low-cost step with potentially high payoff. As Bajaj and colleagues emphasize, integrating simple blood-based indices like the FIB-4 into routine cognitive assessments could flag treatable contributors to decline.
Expert Insight
"When we evaluate memory loss, we often focus entirely on the brain. But the body is a system — the liver’s role in clearing toxins and balancing metabolism directly shapes cognition," says Dr. Elena Vargas, a clinical neurologist and cognitive disorders specialist. "Asking a few extra questions about liver risk factors and ordering basic liver indices can change a patient’s trajectory from irreversible decline to meaningful recovery."
Looking ahead, broader awareness, improved screening protocols, and equitable access to liver disease care could reduce the fraction of misdiagnosed dementia while opening therapeutic pathways for people whose cognitive symptoms are driven by treatable systemic disease. For clinicians and families alike, the take-home message is simple: thinking beyond the brain can save cognition.
Source: sciencealert
Comments
datapulse
FIB-4 flags in 13% seems high. Is that score enough to claim misdiagnosis? I'd want imaging, follow ups, more evidence not just one index
bioNix
Wow, liver causing 'dementia'? That's wild. My uncle improved after liver care, and family thought it was hopeless... eye-opener, really

Leave a Comment