6 Minutes
Tiny lab-grown brain models are giving researchers a new window into psychiatric disorders. By measuring faint electrical signals in pea-sized organoids, scientists have started to distinguish subtle neural communication patterns linked to schizophrenia and bipolar disorder — differences that don’t show up as obvious structural damage. Here’s what that could mean for diagnosis and personalized treatment.
Why organoids matter: a new model for mysterious illnesses
Schizophrenia and bipolar disorder affect millions worldwide, yet their biological fingerprints remain elusive. Unlike Parkinson’s disease, where clinicians can measure dopamine-related changes, psychiatric diagnoses still rely heavily on behavioral assessment and clinical interviews. That uncertainty leads to long cycles of trial-and-error medication adjustments.
Organoids — small, three-millimeter clusters of lab-grown brain tissue derived from a patient’s own cells — offer an experimental bridge. Made from reprogrammed blood or skin cells turned into stem cells, these miniature neural tissues can develop cell types and wiring reminiscent of the human prefrontal cortex. That’s the brain region most closely tied to planning, decision-making and complex cognition.
How researchers listened to tiny brains
In a recent study published in APL Bioengineering, a Johns Hopkins University team led by biomedical engineer Annie Kathuria recorded neural activity from organoids created from people with schizophrenia, people with bipolar disorder, and healthy controls. The organoids were placed on microchips fitted with multi-electrode arrays — effectively a scaled-down electroencephalogram (EEG) that captures electrical spikes, rhythms and timing across the tissue.
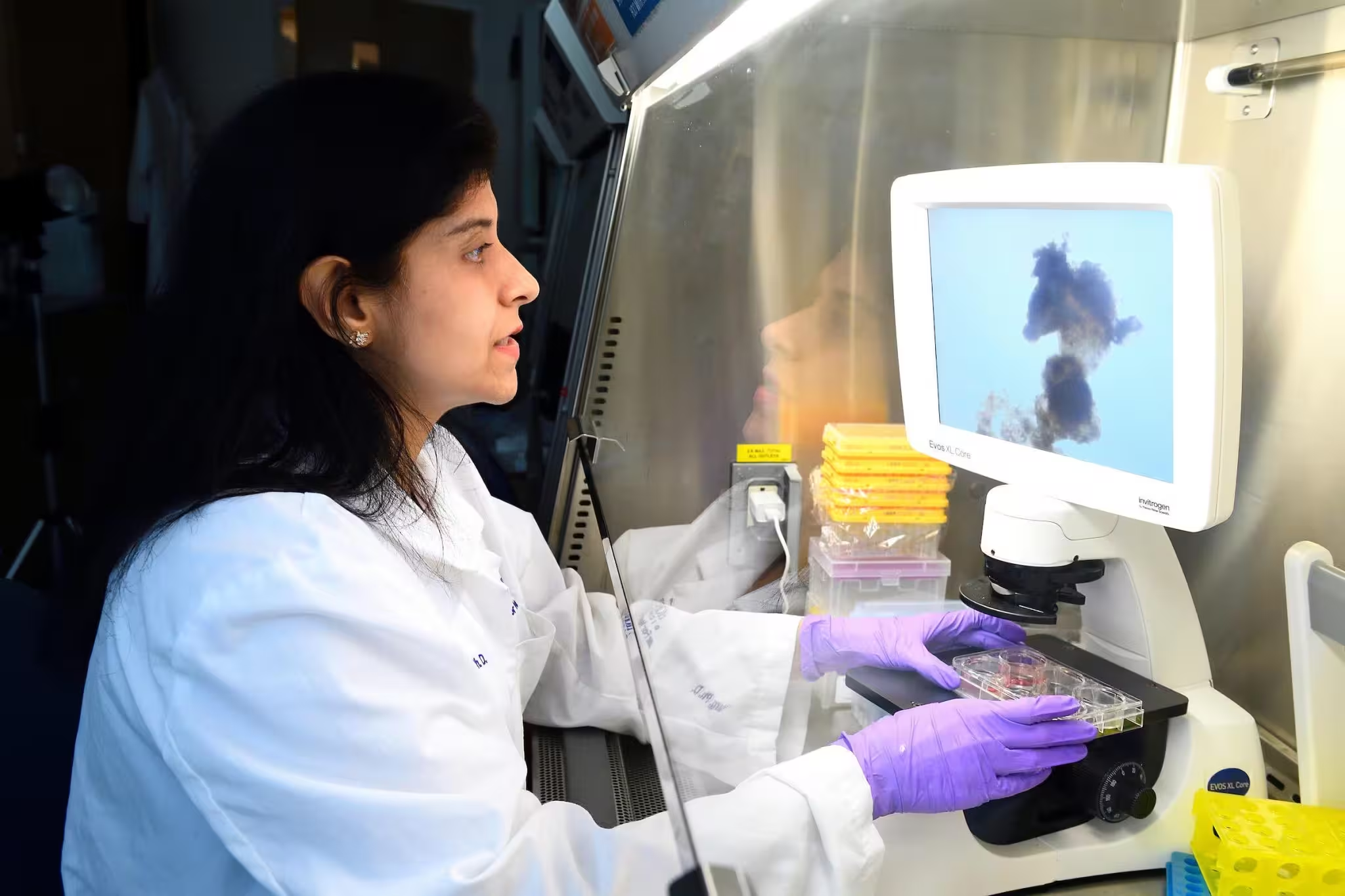
Annie Kathuria
Rather than searching for obvious structural defects, the team focused on electrophysiology: the timing, pattern and coordination of the electrical signals neurons use to communicate. They paired these recordings with machine learning algorithms that could detect subtle, multidimensional patterns across many signal features simultaneously.
Distinct electrical signatures for different disorders
The analysis revealed that organoids derived from schizophrenia and bipolar patients produced unique combinations of firing rates, spike timing and coordinated network behavior. These signatures were not single-point biomarkers but complex profiles — changes across multiple parameters that together acted like a diagnostic fingerprint.
Using these electrophysiological features, the researchers were able to classify the origin of organoids with about 83% accuracy. When they applied gentle electrical stimulation to elicit additional responses, classification jumped to approximately 92% — a strong signal that the neural dynamics themselves carry disorder-specific information.
What this could mean for patients and clinicians
Although the initial study included samples from only a dozen patients, the implications are significant. If validated in larger cohorts, organoid electrophysiology could reduce diagnostic uncertainty and shorten the time patients spend trying multiple medications. Instead of months of trial-and-error, clinicians might one day test drugs directly on a patient’s organoids to predict which treatments normalize the tissue’s electrical patterns.
For example, clozapine is a common antipsychotic prescribed for schizophrenia, but roughly 40% of patients are resistant. Organoid-based drug screening could reveal which patients are unlikely to respond to clozapine and suggest alternative therapies or dosing strategies before exposing the patient to ineffective medications and side effects.
Technical context: microchips, myelin and machine learning
The organoids in this work contain a variety of neural cell types, including myelin-producing cells that speed signal transmission — an important feature because myelination affects timing and coordination in neural networks. The microelectrode arrays act like a grid of tiny sensors, creating a high-resolution dataset. Machine learning models then sift through hundreds of signal features to find consistent patterns that human analysis might miss.
Combining electrophysiology with patient-derived organoids is part of a wider trend in neuroscience: integrating advanced culture methods, microelectronics, and computational analysis to probe brain function at scales between single cells and whole-brain imaging.
Clinical pipeline and next steps
Kathuria’s team is partnering with neurosurgeons, psychiatrists and other neuroscientists at Johns Hopkins School of Medicine to recruit more patients and expand the organoid library. Future experiments will test panels of psychiatric drugs at varying concentrations to see how each treatment shifts the organoid’s electrical fingerprint toward a healthy state. Such a platform could become a preclinical testbed for personalized psychiatry.
Expert Insight
“This approach changes how we think about mental illness,” says Dr. Miriam Santos, a clinical neuroscientist not involved in the study. “Instead of looking for a single mutated gene or a lesion, we can now measure dynamic network dysfunction in tissue derived from individual patients. It’s an essential step toward precision psychiatry, where treatment is informed by the patient’s own neural physiology.”
Broader implications and limitations
While promising, organoid studies have limits. Organoids are simplified models and lack full brain architecture, blood vessels, and long-range connectivity. Small sample sizes can also produce overfitting in machine learning models, so larger, diverse cohorts are essential. Still, this method shines a light on the neural computations that go awry in psychiatric disorders and opens practical routes for drug testing and biomarker development.
As the field advances, integrating organoid electrophysiology with genetics, imaging, and clinical data could produce multi-modal biomarkers powerful enough to guide faster, safer, and more effective psychiatric care.
Source: scitechdaily
Comments
mechbyte
Wait, 83% then 92% with stimulation? sounds promising but is that overfitting? tiny n=12 worries me.
bioNix
Whoa this blew my mind. Tiny organoids showing disease patterns? If real, huge for patients but skeptcal about small samples…


Leave a Comment