6 Minutes
New analysis from the Mayo Clinic challenges a long-held assumption about heart attacks in younger adults: in women under 65, more than half of myocardial infarctions are driven by causes other than the classic blocked artery. That shift has big implications for diagnosis, prevention, and follow-up care.
What the study found and why it matters
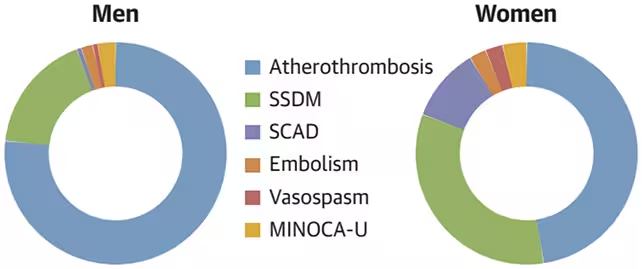
Researchers reviewed 1,474 heart attack events recorded between 2003 and 2018 in Olmsted County, Minnesota, carefully re-examining medical records and cardiac imaging to assign a primary cause to each event. The results were striking: while atherothrombosis — the process where a ruptured plaque triggers a clot that blocks a coronary artery — still accounted for most heart attacks in men (about 75%), it explained only 47% of events in women under 65.
Instead, a large share of women's heart attacks were linked to non-atherothrombotic mechanisms. The single biggest category in women was supply-demand mismatch secondary myocardial infarction (SSDM), responsible for roughly 34% of female cases. SSDM occurs when the heart muscle's oxygen needs exceed supply because of another acute stressor such as severe anemia, sepsis, or respiratory failure.
Other important non-atherothrombotic causes included spontaneous coronary artery dissection (SCAD) — where an artery wall tears and blood collects between layers — and embolisms, in which clots formed elsewhere travel and lodge in a coronary vessel. The team also identified coronary spasm and MINOCA (myocardial infarction with non-obstructive coronary arteries) as contributors.
Age and sex differences: a different landscape for younger women
Sex-based differences were especially clear in the youngest group. Among women aged 45 or younger, SSDM was the most common cause of heart attack. The researchers note that when all acute non-atherothrombotic coronary causes — SCAD, embolism, spasm and undefined MINOCA — are combined, they’re about as common as atherothrombosis in this demographic.
Importantly, many SCAD events were initially misdiagnosed as atherothrombosis. The study found that SCAD was the underlying cause nearly six times more often in women than previously appreciated, which means these patients may have received treatments intended for plaque rupture — therapies that can be ineffective or even harmful when the true problem is an artery wall tear.
Implications for treatment and prevention
When the mechanism of injury is misunderstood, secondary prevention strategies can miss the mark. Standard protocols targeting plaque stabilization and antiplatelet therapy are essential for atherothrombotic heart attacks, but they don’t address the triggers that cause SSDM or the vessel fragility behind SCAD. That mismatch can affect medication choices, intervention strategies and follow-up testing.
The study also linked SSDM with higher five-year all-cause mortality compared with other causes, suggesting these patients often have serious non-cardiac illnesses driving both the heart event and later deaths. That underlines the need for holistic care that treats both the cardiac episode and the broader medical problems contributing to it.
Screening gaps: why risk scores aren’t enough
Current screening tools may further obscure the risk. In a separate analysis cited by the authors, 465 people under 65 who later had a first heart attack were evaluated: two days before their event, nearly 45% would have been classified as low or borderline risk by an ASCVD (atherosclerotic cardiovascular disease) score. In other words, routine risk calculators geared toward atherothrombotic disease can miss many people who go on to have heart attacks driven by other mechanisms.
Clinicians and patients alike need to recognize that a low traditional risk score does not rule out other, potentially serious causes of myocardial infarction — especially in younger women.
What clinicians should look for
- Consider SSDM in patients with acute systemic stress (severe infection, major bleeding, hypoxia) who develop cardiac ischemia despite non-obstructed coronary arteries.
- Raise suspicion for SCAD in younger women presenting with acute coronary syndrome, especially when angiography shows arterial dissections or atypical patterns.
- Evaluate embolic sources (atrial fibrillation, deep vein thrombosis with paradoxical embolus) if coronary occlusion doesn’t fit plaque rupture.
- Use advanced cardiac imaging and multidisciplinary review for ambiguous cases to avoid misclassification and inappropriate therapies.
Expert Insight
"This study is a wake-up call," says Dr. Elena Martinez, a cardiologist and clinical researcher who was not involved with the Mayo Clinic analysis. "We’ve long relied on the atherothrombotic model because it explains a large fraction of heart attacks, but younger women present differently. If clinicians default to the plaque-rupture explanation, they may miss treatable non-coronary causes and fail to tailor prevention strategies. Better imaging, careful history-taking, and awareness of entities like SCAD and SSDM can change outcomes."
Where research and practice should go next
The Mayo Clinic team calls for increased clinician awareness and public education about alternative heart attack causes. They also recommend applying their detailed adjudication approach across larger, more diverse populations to better understand sex and age differences, and to refine diagnostic pathways that reduce misdiagnosis.
Improvements in cardiac imaging over the study period likely made some of these diagnoses more visible, and continued technological progress should help. Meanwhile, researchers and professional societies will need to update guidelines and training so cardiologists, emergency physicians and primary care clinicians can recognize non-atherothrombotic presentations early.
Understanding why a heart attack happened is as important as treating it. For younger women, that understanding may mean different tests, different medicines and, crucially, different conversations about risk and recovery.
The study was published in the Journal of the American College of Cardiology; an earlier version of this article appeared in September 2025.
Source: sciencealert
Comments
Reza
Is this even true? 45% labeled low risk then a heart attack 2 days later, sounds off. Need larger, diverse studies before revamping care
atomwave
Wow, I had no idea. Younger women get so many non-plaque MIs… SCAD and SSDM way more common than I thought. Risk scores can lie, scary

Leave a Comment