4 Minutes
New long-term research suggests that returning fasting blood sugar to normal — not the number on the scale — is the most important target in preventing type 2 diabetes. Lifestyle changes focused on diet and exercise cut diabetes risk dramatically, even when weight loss is minimal.
What the study looked at and why it matters
An international team followed 1,105 people with prediabetes who enrolled in a 12-month lifestyle program emphasizing healthier eating and increased physical activity. Researchers tracked participants for up to 10 years to see who progressed to type 2 diabetes.
After one year, 234 participants had not lost weight. Of those, 51 achieved what the team defined as prediabetes remission — their fasting blood glucose returned to a normal range. Over the long follow-up, that subgroup was about 71% less likely to develop type 2 diabetes than the 183 people who remained glucose-impaired despite also not losing weight.
The protective effect was nearly identical to the benefit seen in participants who did lose weight and reached remission (a roughly 73% reduction in risk compared with those who lost weight but did not remit). The results were published in Nature Medicine (Sandforth et al., Nat. Med., 2025).
Why blood glucose control can beat the scale
Researchers point to where fat is stored as a key factor. A subset analysis showed that people who normalized fasting glucose without losing weight had lower levels of visceral fat — the metabolically active fat that surrounds organs — than those whose blood sugar stayed high. Visceral fat is strongly linked to insulin resistance, a major driver of type 2 diabetes.
“Restoring a normal fasting blood sugar level is the most important goal in preventing type 2 diabetes and not necessarily the number on the scale,” says diabetologist Andreas Birkenfeld of the University of Tübingen. “Exercise and a balanced diet have a positive effect on blood sugar levels, regardless of whether weight is reduced.”
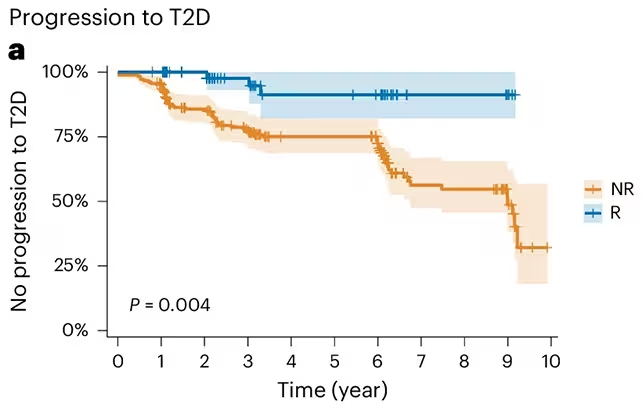
Those who had reached prediabetes remission (R) were less likely to develop type 2 diabetes compared to those who hadn't (NR), even without weight loss.
Implications for treatment and public health
The authors argue that current guidelines, which often emphasize body mass or weight loss as primary endpoints, may need updating. Focusing predominantly on weight can discourage people who benefit metabolically from lifestyle changes but struggle to shed pounds.
“In the future, guidelines for the prevention and treatment of type 2 diabetes should not only take weight into account, but above all blood glucose control and fat distribution patterns,” says Reiner Jumpertz-von Schwartzenberg, also of the University of Tübingen.
That shift would place greater value on measurable improvements in fasting glucose and on interventions known to reduce visceral fat — such as regular aerobic exercise, resistance training, and dietary patterns that lower liver fat and improve insulin sensitivity.
Practical takeaways for people with prediabetes
- Target fasting glucose and HbA1c improvements alongside weight goals — returning blood sugar to normal is a clear, evidence-backed objective.
- Focus on exercise and dietary quality: these interventions can reduce visceral fat and improve insulin sensitivity even without large changes in body weight.
- Regular monitoring matters: early remission of prediabetes predicts a much lower long-term risk of progressing to type 2 diabetes.
This study does not negate the benefits of weight loss for many people, but it reframes prevention: metabolic health and fat distribution can be stronger predictors of future diabetes risk than weight alone. Clinicians and guideline writers may need to consider more nuanced targets — and patients can take heart that measurable blood-sugar improvements count, even when the scale moves slowly.
Source: sciencealert


Leave a Comment