4 Minutes
Scientists have begun to tease a reliable signal out of the brain’s electrical “static” that maps directly onto Parkinson’s movement problems. By pooling deep-brain recordings from dozens of patients, researchers say they can now identify rhythmic patterns that may one day guide adaptive therapies and improve motor control.
Listening for meaning in the brain’s noise
Parkinson’s disease arises when the basal ganglia — a network deep in the brain that helps filter and coordinate movement — stops working properly. The result is the familiar trio of slowed movement, stiffness and tremor. For years scientists have observed increases in certain electrical rhythms, especially mid-to-high-frequency oscillations called beta waves, in patients’ basal ganglia. But those signals were noisy, inconsistent across studies, and hard to match to specific symptoms.
Researchers at the Max Planck Institute for Human Cognitive and Brain Sciences led an international effort to change that. They combined five separate sets of electrophysiological recordings taken from deep-brain electrodes implanted in 119 people with Parkinson’s disease. Rather than comparing sick brains to unrelated control subjects, the team compared activity between the two hemispheres within each person — a tactic that helps isolate disease-related rhythms from individual variability.
"You can imagine the brain as a concert hall full of musicians before a rehearsal," neurologist Moritz Gerster, the study's lead author, explained. “Some groups play together, creating a distinct rhythm. Others practice on their own, merging into a non-rhythmic 'noise'. If you only measure the overall volume, you miss this distinction.”
How the signal maps onto movement
By separating rhythmic activity from non-rhythmic firing, the team found consistent patterns of beta-band oscillations and spiking activity that correlated with the severity of motor impairments. In short: particular rhythms deep in the basal ganglia reliably reflected how impaired a patient’s movements were.
That matters because current deep brain stimulation (DBS) — an established therapy for some people with Parkinson’s — typically delivers continuous electrical pulses. If clinicians can instead monitor the brain in real time and stimulate only when pathological rhythms emerge, therapy could become both more precise and more effective. Imagine a conductor who finally knows which instruments are out of time and nudges them back into rhythm.
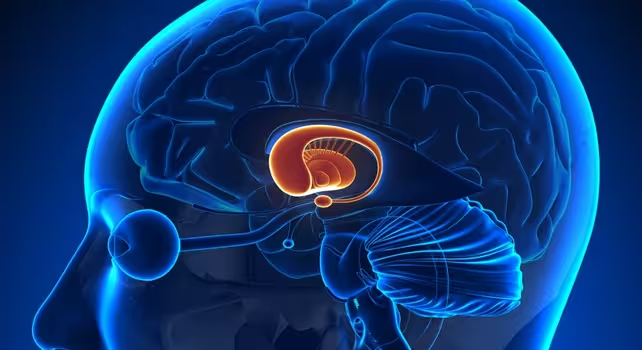
Location of the basal ganglia in the brain
Implications for treatment and research
The study’s approach — pooling datasets and using within-patient hemisphere comparisons — reduces confounding factors like patient diversity and mixed symptom profiles. That makes the identified rhythms stronger candidate biomarkers for adaptive neuromodulation systems. Developers of next-generation DBS devices could use these biomarkers to trigger stimulation only when pathological activity appears, potentially improving motor outcomes and reducing side effects.
Publishing their results in eBioMedicine, the team suggests these electrophysiological markers could also help refine clinical trials, accelerate device testing, and tailor therapies to the fluctuating needs of individual patients.
What’s next?
Translating these findings into everyday care will require clinical trials that test rhythm-driven stimulation protocols and long-term monitoring to confirm benefits. But by showing a dependable signature of Parkinson’s motor dysfunction buried in the brain’s electrical background, the study brings adaptive neuromodulation a meaningful step closer.
For clinicians, engineers and patients alike, the discovery raises a hopeful possibility: rather than treating Parkinson’s with blunt, continuous pulses, we may soon be able to tune stimulation to the brain’s own rhythms — improving quality of life by listening before acting.
Source: sciencealert


Leave a Comment