3 Minutes
Researchers at MIT have engineered nanoparticles that deliver the immune-activating molecule interleukin‑12 (IL‑12) directly into ovarian tumors, dramatically improving immunotherapy outcomes in mice. The approach reduces systemic toxicity while energizing local immune cells — and in combination with other drugs it cleared metastatic ovarian cancer in over 80% of treated animals.
Why ovarian cancer resists current immunotherapies — and how IL‑12 changes the game
Ovarian cancer is one of the most treatment‑resistant solid tumors. Tumors often create an immunosuppressive microenvironment that muffles T cells and other immune defenders. Checkpoint inhibitors — drugs that release the "brakes" on immune cells — have revolutionized care for some cancers, but they rarely work against ovarian tumors by themselves.
IL‑12 is a potent cytokine that can reawaken T cells and innate immune populations inside tumors, but systemic delivery at therapeutic doses causes dangerous side effects such as severe inflammation, liver toxicity, and even death. The MIT team sought to keep IL‑12’s potency while avoiding its toxicity by putting it where it matters most: inside the tumor.
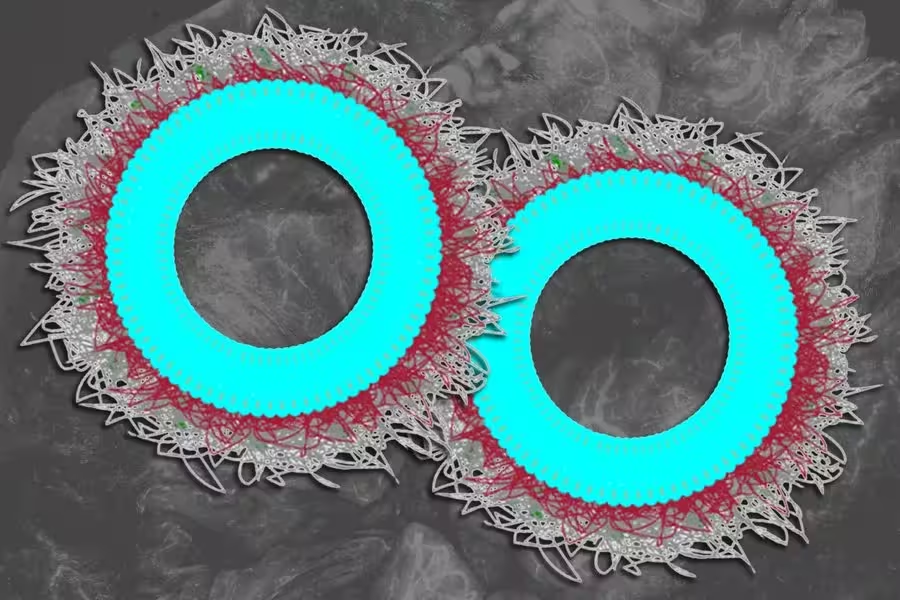
Smart nanoparticles: design, release, and tumor targeting
To do that the researchers attached IL‑12 to tiny lipid droplets called liposomes that are coated with a biodegradable polymer, poly‑L‑glutamate (PLE). A stable chemical linker binds IL‑12 to the liposome so the cytokine is released gradually — over roughly a week — rather than flooding the body all at once. This slow, localized release keeps immune cells engaged in the tumor microenvironment while limiting harmful systemic exposure.
In mouse experiments, the IL‑12 nanoparticle therapy alone cleared tumors in about 30% of animals. But when combined with specific inhibitors and companion drugs that modulate the immune response, cure rates climbed above 80%, including in aggressive or drug‑resistant tumor models.
"The really exciting part is that we delivered IL‑12 directly into the tumor environment," says Paula Hammond, a senior author on the study. "With this nanoparticle design we essentially tricked the cancer into activating the immune system against itself."
Durable immunity and implications for future treatment
Beyond tumor regression, the treatment produced long‑lasting immune memory in mice. Months after successful therapy, researchers reintroduced tumor cells and found that the animals’ immune systems eliminated them before new tumors could establish. That suggests potential not only for tumor clearance but for lasting protection.
The work, published in Nature Materials, points to several future directions: optimizing dosing and combination partners, testing safety and efficacy in larger animal models, and ultimately designing human trials. Translating from mice to patients will require careful assessment of risks and benefits, but the targeted IL‑12 delivery concept addresses a major hurdle in cytokine therapy — systemic toxicity.
What this means for cancer immunotherapy
This MIT study demonstrates that nanoparticle delivery systems can revive powerful but previously unusable immune drugs by localizing their effects. For ovarian cancer — a disease in urgent need of better options — such an approach could reshape how oncologists use cytokines, combining precise drug delivery with modern immunomodulatory regimens.

Leave a Comment