6 Minutes
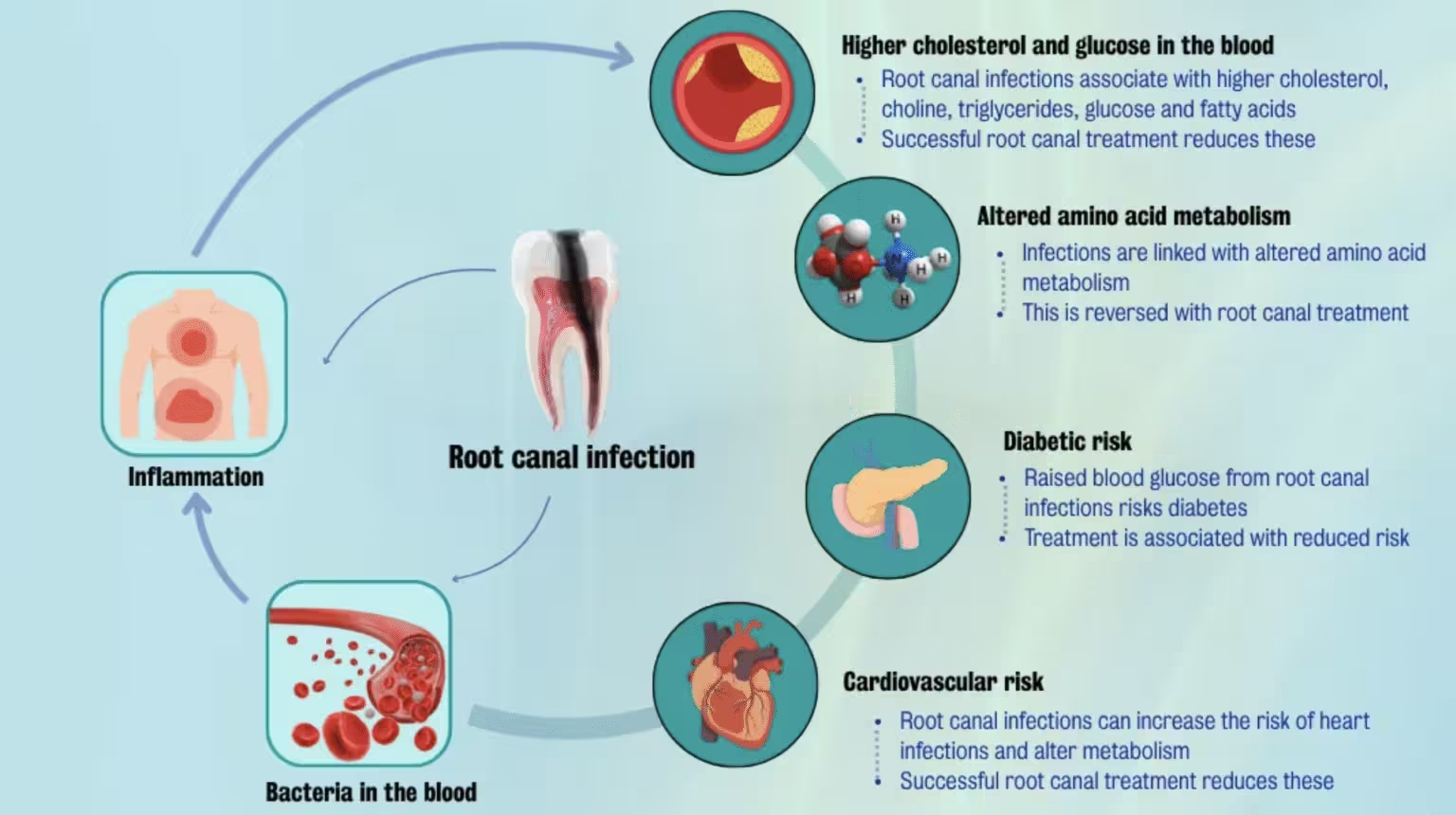
New research suggests that treating chronic root canal infections could improve markers of blood sugar control and reduce systemic inflammation — a finding that links oral health to metabolic and cardiovascular risk in surprising ways.
Small study, big implications: oral infections and your blood chemistry
Researchers at King's College London and the University of Helsinki followed 65 patients with apical periodontitis — a persistent infection at the tip of a tooth root — and tracked changes in their blood over two years after root canal treatment. The team reported “exceptional improvements” in markers of inflammation and metabolism, including a significant fall in serum glucose levels two years after successful treatment.
Although the study was observational and lacked a randomized control group, the results add to a growing body of evidence linking oral microbes and chronic dental infections with systemic disease. If confirmed in larger trials, these findings could shift how clinicians think about dental care, diabetes prevention, and cardiovascular risk management.
How the researchers measured change
To explore the link between infected tooth roots and metabolic health, investigators collected blood samples at five time points: before root canal treatment and at 3 months, 6 months, 1 year, and 2 years post-treatment. They measured 44 metabolites tied to inflammation and metabolism, including amino acids, lipids, glucose, and compounds involved in energy pathways.
Key observations included a short-term drop in cholesterol three months after treatment and an early decline in a group of amino acids associated with insulin resistance. Broader improvements in blood glucose levels emerged later, becoming significant at the two-year mark. The researchers also reported a decline in pyruvate — a metabolic intermediate linked to inflammatory signaling — alongside the glucose improvements.
Why these biomarkers matter
- Serum glucose: Persistent high blood sugar is a major risk factor for type 2 diabetes and increases the chance of heart attacks and stroke.
- Amino acids associated with insulin resistance: Elevated levels can indicate disrupted metabolic processing and predispose patients to hyperglycemia.
- Pyruvate and inflammatory markers: These reflect how infection-driven inflammation may ripple through metabolic pathways.
From mouth to metabolism: a plausible biological link
Apical periodontitis allows bacteria to persist deep inside tooth tissues. Researchers propose that these microbes or their inflammatory signals can enter the bloodstream, triggering systemic immune responses that disturb metabolic balance and insulin sensitivity. That pathway — chronic oral infection causing low-grade systemic inflammation — is biologically plausible and fits with other studies that have found oral bacteria in atherosclerotic plaque.
Lead author and endodontologist Sadia Niazi of King's College London emphasized the broader implications: “Our findings show that root canal treatment doesn't just improve oral health – it may also help reduce the risk of serious health conditions like diabetes and heart disease. It's a powerful reminder that oral health is deeply connected to overall health.”
Still, the team is cautious. Because the trial was observational and without a control arm, causation cannot be established: successful root canal therapy may coincide with other health behaviors or interventions that contributed to improved metabolic markers.
Clinical and public-health implications
If future randomized trials confirm that resolving chronic dental infections improves metabolic outcomes, the implications are wide-ranging. Dentists could play a more proactive role in chronic disease prevention; primary care doctors might monitor dental inflammation when assessing cardiovascular or diabetes risk; and healthcare systems could integrate oral and medical records to identify patients at higher systemic risk due to untreated dental infections.
Some epidemiological estimates already suggest that people with infectious lesions around their teeth may have more than double the risk of coronary artery disease later in life. This study reinforces the idea that oral health is not isolated: it may be an early, modifiable factor in the cascade toward metabolic disease.
Expert Insight
“This study is an important signal that chronic dental infections can have measurable effects beyond the mouth,” says Dr. Miriam Holt, a clinical epidemiologist specializing in inflammation and chronic disease. “The metabolic shifts reported here — declines in amino acids tied to insulin resistance and a delayed drop in serum glucose — are consistent with a model in which prolonged immune activation nudges metabolism toward dysfunction. We need randomized studies, but the message for now is practical: treat chronic dental infections promptly and consider oral health when evaluating metabolic risk.”
What’s next for research and care?
The authors call for larger, controlled trials to test whether root canal therapy directly causes metabolic improvement or whether the observed associations reflect confounding factors. They also argue for integrated care models: dental professionals working with general practitioners to monitor blood markers and manage patients holistically.
For patients and clinicians alike, the takeaway is straightforward: oral infections are not merely a dental problem. They may contribute to systemic inflammation and metabolic changes that matter for diabetes and heart disease risk. Paying attention to dental infections — and treating them promptly — could be a small but meaningful step toward better overall health.
Source: sciencealert
Comments
atomwave
Wait, only 65 patients and no control group? Sounds promising but is this causal or just coincidence? More trials pls, science needs rigour...
bioNix
Wow never thought a root canal could change blood sugar. Mind blown, kinda alarming actually. If fixing teeth trims diabetes risk thats huge — but wait, need more proof.


Leave a Comment