6 Minutes
New genetic research links common blood-group variants to a modest change in the chance of having a stroke before age 60. The study highlights how inherited biology — something you can't change — may shift risk in subtle but measurable ways.
Blood groups, genes and a surprising signal
Most people know the ABO groups — A, B, AB and O — as the labels used for transfusions. These categories reflect antigens: chemical markers on the surface of red blood cells. But those broad groups hide smaller genetic variations. A team of international researchers pooled data from 48 genetic studies to ask whether any of those variations are linked to early-onset ischemic stroke, the kind caused by blocked blood vessels in the brain.
Across roughly 17,000 people who had experienced a stroke and nearly 600,000 controls (all aged 18–59), the genome-wide analysis pointed to two locations in the genome strongly associated with stroke risk. One of those locations overlapped the ABO blood-group locus — the stretch of DNA that determines A, B and O antigens.
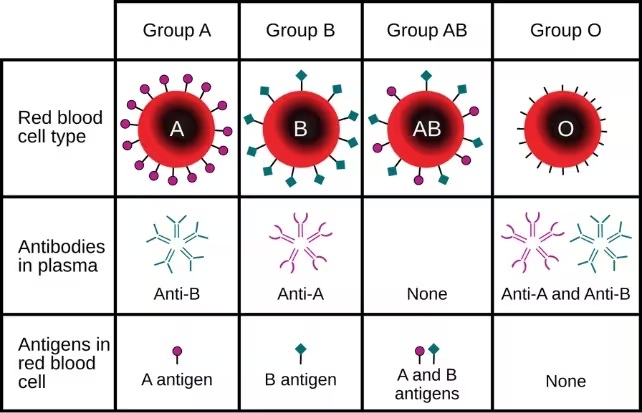
Blood type is partly determined by the ABO blood group antigens present on red blood cells.
What the data showed: small but measurable differences
When the team dug deeper into blood-type subgroups, an A1 genetic signature stood out. Individuals whose DNA coded for the A1 subgroup had about a 16% higher risk of stroke before age 60 compared with people with other blood-type genotypes. Conversely, the O1 genetic variant was associated with a roughly 12% lower risk.
The study also reported that people with type B genetics faced an approximately 11% higher stroke risk compared with non-stroke controls regardless of age. Those changes in risk are modest at the individual level, but because blood type is common and easily measured, the finding has population-level relevance.
Why might blood type affect stroke?
Researchers do not yet have a definitive biological explanation, but many hypotheses center on blood-clotting and vascular biology. Genomic signals at the ABO locus have previously been linked to venous thromboembolism (blood clots in veins), coronary calcification and heart attack. That suggests the ABO region affects circulating proteins, platelet activity or the cells that line blood vessels — all contributors to clot formation.
Senior author Dr. Steven Kittner from the University of Maryland noted the clinical importance of studying early strokes: these events are growing in number and can cause long-lasting disability or death. Unlike late-onset strokes, which are often driven by atherosclerosis — the slow buildup of fatty plaques in arteries — strokes in younger adults are more frequently associated with clotting and other non-atherosclerotic mechanisms.
Study scope, limits and why the risk remains small
The researchers were careful to put their findings in context. Although millions of people in the U.S. experience stroke each year, most events occur after age 65. The additional percentage points of risk associated with an A1 genotype are statistically meaningful but clinically modest; the authors say there is currently no reason for people with A blood type to seek extra screening solely on that basis.
Geographic and ancestral coverage also matters. Participants came from North America, Europe, Japan, Pakistan and Australia, but only about 35% were of non-European ancestry. Greater diversity in future studies will be essential to confirm how broadly the associations apply.
To compare age effects, the team also looked at data from about 9,300 stroke cases over age 60 and roughly 25,000 older controls. In that late-onset group, the A1 association disappeared, reinforcing the idea that early and late strokes can have different biological drivers.
Implications for patients and clinicians
For clinicians, the takeaway is twofold: first, genetics can help reveal pathways that drive disease, suggesting new targets for research and therapy; second, modest population-level associations should not be overinterpreted into individual medical advice. Lifestyle factors, blood pressure control, smoking cessation and management of diabetes remain central to stroke prevention.
Co-author Mark Gladwin (University of Maryland) emphasized that this research expands our knowledge about non-modifiable risk factors and provides clues rather than clinical directives. Continued work is needed to tease apart which blood proteins or vascular processes are altered by ABO variants and whether those pathways are actionable.
Next steps in research
- Replicate findings in more diverse populations to test consistency across ancestries.
- Perform functional studies to identify the proteins or cells affected by ABO variants.
- Explore whether combining genetic risk with established risk factors improves early-stroke prediction models.
Expert Insight
"This study is a clear example of how genetics can point us toward biology we might otherwise overlook," says Dr. Elena Moran, a vascular neurologist and genomics researcher not involved in the paper. "The effect sizes are modest, but the ABO signal is reproducible across several vascular traits. Understanding the molecular link between blood-group chemistry and clotting could open new preventive strategies — especially for younger adults whose strokes are often driven by clotting rather than plaque buildup."
Where the evidence stands today
The research, published in Neurology in 2022, adds an important piece to the puzzle of early-onset stroke. It shows that common, inherited differences in blood-group genes can slightly alter stroke risk in younger adults, likely through clotting-related mechanisms. But this is a first step: broader samples, functional assays and deeper clinical integration will be needed before blood type becomes part of routine stroke risk screening.
Source: sciencealert
Comments
skyspin
So A1 up ~16% but really, is that clinically useful? Study mostly Europeans, need more diverse samples, not sold yet
bioNix
Whoa, A1 blood linked to early stroke? That’s kinda scary… never knew type mattered so much, hmm

Leave a Comment