5 Minutes
New international research shows that many psychiatric diagnoses share a common genetic architecture. By comparing DNA from more than a million people with 14 different mental-health diagnoses to several million controls, scientists uncovered recurring genetic patterns that help explain why multiple disorders often appear together.
How the study mapped shared genetic risk
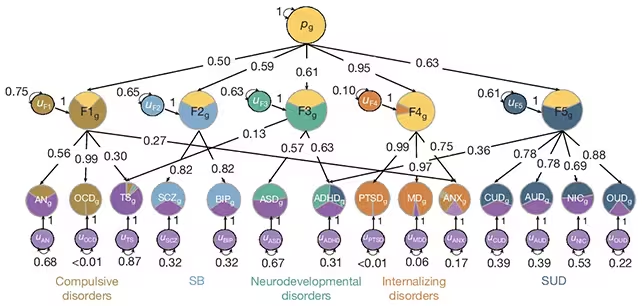
An expansive team of researchers pooled genome data from over 1 million diagnosed cases and roughly 5 million controls to look for overlapping genetic signals across 14 psychiatric disorders. Using statistical models that detect correlated genetic variation across conditions, the group identified five robust genomic factors—clusters of genetic variants that recur across diagnoses. In total, these five factors are composed of 238 genetic variants and explain, on average, about two-thirds of the genetic differences between people with psychiatric disorders and those without.
Instead of thinking of each diagnosis as genetically distinct, the analysis grouped conditions by the genetic signatures they share. That approach reveals how biology bridges diagnoses that clinicians traditionally separate by symptoms alone.
Five genetic patterns—five clinical clusters
Each genomic factor aligned strongly with a recognizable cluster of disorders:
- Compulsive disorders, such as obsessive-compulsive disorder (OCD).
- Internalizing disorders, including major depression and anxiety.
- Substance use disorders.
- Neurodevelopmental conditions, like autism spectrum disorders.
- A combined bipolar disorder and schizophrenia cluster.
Perhaps most strikingly, the bipolar–schizophrenia cluster shared roughly 70% of its genetic signaling between the two conditions. "Genetically, we saw that they are more similar than they are unique," says neuroscientist Andrew Grotzinger of the University of Colorado Boulder. That high degree of overlap helps explain why co-occurrence and diagnostic crossover are common in clinical practice.
Biology behind the overlap: early brain development and cell types
Beyond grouping disorders, the researchers traced the shared variants to biological pathways that could be clinically meaningful. Some risk variants map to genes involved in early brain development and neuron signaling—processes fundamental to how the brain wires itself. Variants tied to bipolar disorder and schizophrenia were enriched in genes active in excitatory neurons, while the depression/anxiety cluster showed links to oligodendrocytes, the supportive cells that insulate and metabolically support neurons.
These cellular clues suggest that the same developmental or signaling disruptions can manifest as different psychiatric symptoms depending on timing, environment, or additional genetic factors. That helps explain why a single person may receive multiple psychiatric diagnoses over time.
Clinical implications and the road ahead
The new genetic map won't change how clinicians diagnose patients tomorrow, but it provides a clearer biological framework for future practice. If disorders once treated completely separately are driven by shared biology, treatments could be redesigned to target common pathways—reducing polypharmacy and simplifying therapy plans for people with multiple conditions. "By identifying what is shared across these disorders, we can hopefully come up with ways to target them in a different way that doesn't require four separate pills or four separate psychotherapy interventions," Grotzinger adds.
Researchers emphasized the need to expand analyses to larger and more diverse populations. Most current genome studies are heavily weighted toward people of European ancestry, which limits how broadly findings can be applied. The team also highlighted that translating genetic signals into safe, effective treatments requires careful laboratory work to understand mechanisms, then clinical trials to test interventions.
Expert Insight
Dr. Emily Harper, a clinical geneticist and science communicator, notes: "This study gives us a practical lens on psychiatric comorbidity. When we see overlapping genetic architecture, it encourages a precision-medicine approach—one that blends genetics, developmental neurobiology and patient-centered care. The challenge now is converting statistical signals into interventions that help real patients across diverse communities."
Published in Nature (Grotzinger et al., 2025), the study points to a future where diagnosis and treatment consider shared genetic roots alongside symptoms—offering a more integrated view of mental health that could improve outcomes for millions.
Source: sciencealert
Comments
Reza
Is this even true? 70% overlap sounds high. Are environmental factors accounted for, or is it just statistical correlation? curious but skeptical.
atomwave
wow, kinda mind blown. genetics linking so many disorders… if true this could change treatment, but we need more diversity in samples, pronto

Leave a Comment