8 Minutes
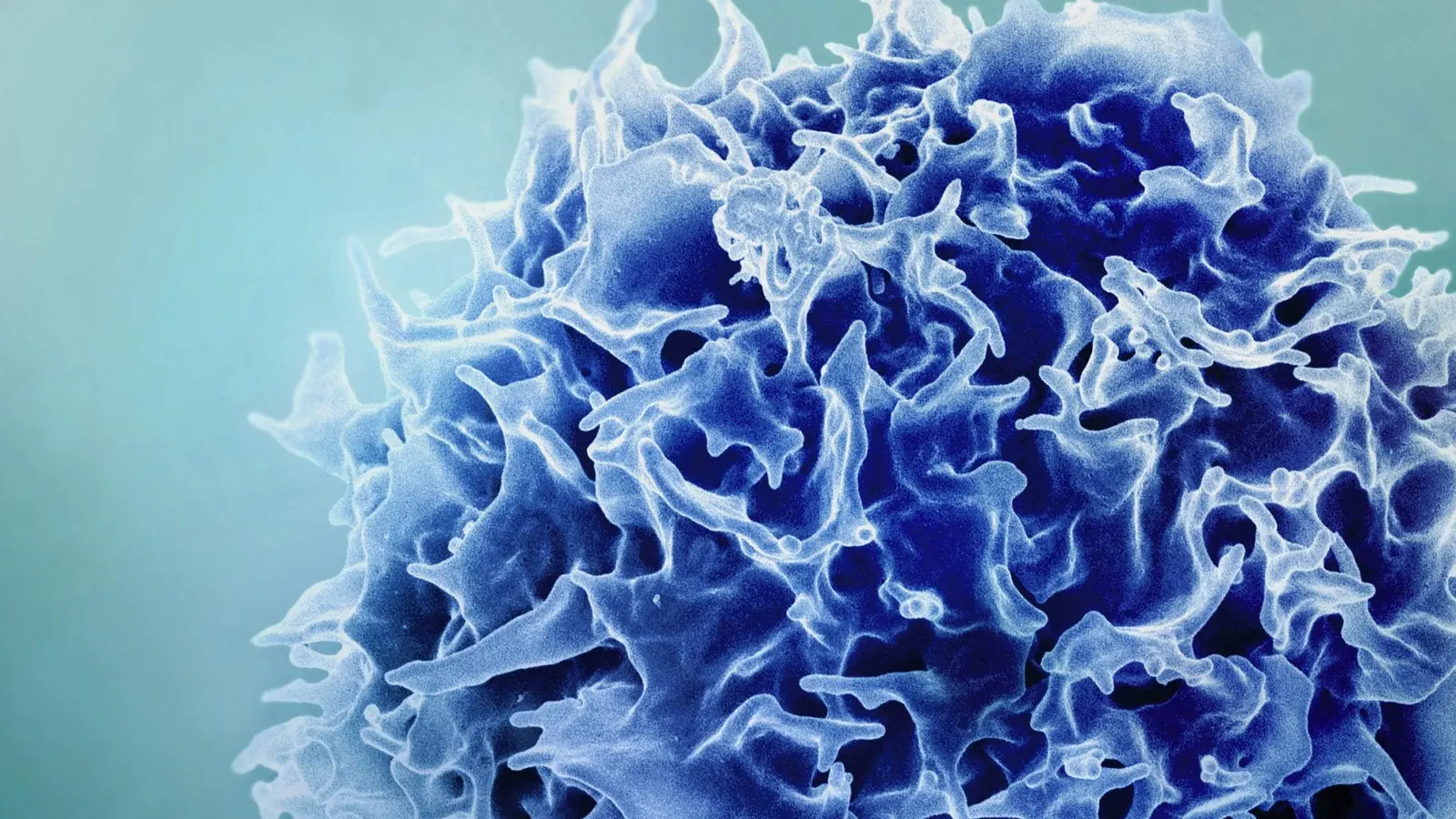
Researchers at MIT and the Broad Institute have developed a novel way to temporarily revive aspects of the aging immune system by reprogramming the liver to produce signals normally secreted by the thymus. Using short-lived mRNA delivered in lipid nanoparticles, the team prompted liver cells to support T-cell maturation, improving vaccine responses and boosting cancer immunotherapy in mice.
Encouraging the liver to generate certain signals normally produced by the thymus can help counteract age-related reductions in T-cell numbers and improve how well the immune system responds to vaccines.
Turning the liver into a temporary immune factory
The thymus — a small gland in front of the heart — is the body’s primary site for T-cell development. As immature T cells pass through the thymus they are vetted, shaped, and released as a diverse pool of mature T cells able to recognize a wide array of pathogens and abnormal cells. But starting in early adulthood the thymus progressively shrinks, a process called thymic involution. By roughly age 75 the organ is effectively nonfunctional in many people, and the supply of new T cells drops.
Instead of attempting to regrow or transplant thymic tissue, the MIT team asked a different question: could another organ be temporarily reprogrammed to produce the same signals that the thymus normally secretes? The liver emerged as an attractive candidate. It tolerates protein production well even in older individuals, it receives a huge fraction of the body’s blood flow (including circulating immune progenitors), and delivering mRNA to hepatocytes via lipid nanoparticles is already a practical route in the clinic.
"Our approach is more of a synthetic approach," said Feng Zhang, the senior author of the study and a professor at MIT. "We're engineering the body to mimic thymic factor secretion."
How the mRNA therapy works
The team encoded three critical thymic cues — DLL1, FLT-3 ligand, and interleukin-7 (IL-7) — into mRNA molecules packaged inside lipid nanoparticles. When injected into the bloodstream, these nanoparticles preferentially accumulate in the liver, where hepatocytes take up the mRNA and translate it into proteins. Because mRNA is inherently transient, the liver functions as a temporary factory, secreting the factors for a limited time rather than permanently altering cells.
Why those three factors?
- DLL1 contributes to Notch signaling, a pathway essential for commitment of progenitors to the T-cell lineage.
- FLT-3 ligand supports the survival and expansion of early progenitor cells.
- IL-7 is a well-known cytokine that promotes T-cell survival, proliferation, and homeostasis.
Delivering all three in combination recapitulates multiple aspects of the thymic environment that single factors alone cannot reproduce, the researchers report.
Evidence of immune rejuvenation in aged mice
To test their concept, the scientists treated 18-month-old mice (roughly equivalent to humans in their 50s) with repeated injections of the mRNA formulation over a four-week period. Because the mRNA effect is short-lived, multiple doses were required to sustain production while new T cells matured.
After treatment, the treated mice showed larger and more diverse T-cell populations. When vaccinated with a model antigen (ovalbumin), older mice that had received the liver-directed mRNA produced roughly double the number of cytotoxic T cells specific to that antigen compared to untreated peers. That translated into a stronger and more focused vaccine response.
The team also investigated cancer therapy. Aged mice were implanted with tumors and treated with a PD-L1 checkpoint inhibitor, a drug class designed to lift inhibitory brakes on T cells. Mice that had received the liver mRNA regimen before checkpoint inhibition had substantially higher survival rates and lived longer than those that received the checkpoint inhibitor alone, suggesting improved antitumor immunity.
What this means and what’s next
These results hint at a practical strategy for enhancing immune resilience in older populations — not by permanently editing immune organs but by temporarily supplementing the body with missing developmental cues. The technique relies on modern mRNA delivery platforms, the same modality used in recent vaccine technologies, which may accelerate translational prospects.
Importantly, the researchers found that all three factors were required to generate the full set of benefits; removing any single component reduced efficacy. That observation underscores the complexity of thymic signaling and why single-molecule therapies have had limited success at fully restoring immune function.
Future work will test the approach in additional animal models, probe effects on other immune compartments such as B cells and innate populations, and search for extra signals that might further amplify or refine the response. Safety studies will be essential: prior attempts at systemic delivery of growth factors produced concerning side effects, and any human translation must balance benefit with risk.
"If we can restore something essential like the immune system, hopefully we can help people stay free of disease for a longer span of their life," Zhang said, highlighting the broad potential impact if the method proves safe and effective in humans.
MIT former postdoc Mirco Friedrich, the paper’s lead author, noted that the idea grew from a practical view of organ biology: recruit an organ that can safely and transiently perform a different task rather than attempting complex organ regeneration. "As we get older, the immune system begins to decline. We wanted to think about how we can maintain this kind of immune protection for a longer period of time," he said.
Expert Insight
Dr. Elaine Morrison, an immunogerontologist at a major academic medical center (commenting as an independent expert), said: "This study cleverly repurposes the liver using mRNA technology to deliver a combinatorial signal set that mimics the thymic niche. It is an elegant workaround to thymic involution and could complement vaccines and cancer immunotherapies for older adults — provided clinical safety is established. The transient nature of mRNA expression is a clear advantage here."
Broader implications and related technology
The work sits at the intersection of several contemporary trends: mRNA therapeutics, targeted nanoparticle delivery, and immune rejuvenation. Each of these areas has matured rapidly in the past decade, lowering technical barriers to clinical testing. Because lipid nanoparticle-mediated mRNA delivery is already used in approved vaccines, regulatory pathways and manufacturing expertise exist that could accelerate first-in-human studies.
Beyond aging, temporary reprogramming of organs to emit beneficial signaling molecules could find applications in immune deficiencies, recovery after intensive chemotherapy, or short-term enhancement of vaccine efficacy during outbreaks. However, translating promising mouse results to humans is notoriously challenging: doses, immune dynamics, and safety profiles can differ substantially between species.
The MIT-Broad team plans additional preclinical work to refine dosing, expand the roster of supportive signals, and evaluate long-term consequences on immune homeostasis. If those steps are successful, the approach may enter early clinical trials aimed at bolstering immunity in older adults or other vulnerable groups.
Retaining immune competence with age could reduce susceptibility to infections, improve responses to vaccinations, and enhance the effectiveness of cancer immunotherapies. This study demonstrates a creative, short-term biological engineering strategy that may be part of a future toolkit for healthier aging.
Source: scitechdaily
Comments
bioNix
is this even true? mice to humans is a huge leap, and systemic growth factors had bad side effects before. curious, but skeptical tbh
atomwave
wow didnt expect that... turning the liver into a temporary thymus? mind blown, but kinda uneasy. safety studies gotta be solid asap

Leave a Comment