4 Minutes
Imagine that one-third of a crisis could be stopped before it starts. That is the blunt finding from a sweeping World Health Organization analysis: in 2022 roughly 19 million people were diagnosed with cancer worldwide, and about 38 percent of those cases were tied to risk factors we can change.
Those risk factors are a mix of lifestyle choices, infectious agents, workplace exposures and environmental harms. But two habits stand out. Tobacco smoking remains the single largest preventable driver of cancer — connected to an estimated 15 percent of new diagnoses that year — and alcohol use is the second most important modifiable lifestyle contributor. Put simply: a few widespread behaviors account for a very large slice of the global cancer burden.
Why does this matter? Because prevention, when it works, multiplies benefits. Reducing smoking and hazardous drinking not only lowers lung and liver cancers but also trims risks for stomach, colorectal and other cancers. Add vaccination, cleaner air and safer workplaces to the mix, and the potential drop in new cancer cases becomes substantial.
What the WHO analysis reveals and why regional patterns differ
The WHO team examined 30 changeable risk factors and calculated how many new cancers could be linked to them. The big picture is stark: tens of millions of potentially avoidable cases worldwide. Yet the details vary by place and by sex. For men, smoking accounted for nearly a quarter of new cancers globally in 2022. For women in some regions, air pollution contributed unexpectedly large shares of lung cancer; in East Asia, about 15 percent of female lung cancer cases were linked to polluted air. In Northern Africa and Western Asia, air pollution accounted for roughly one in five male lung cancers.
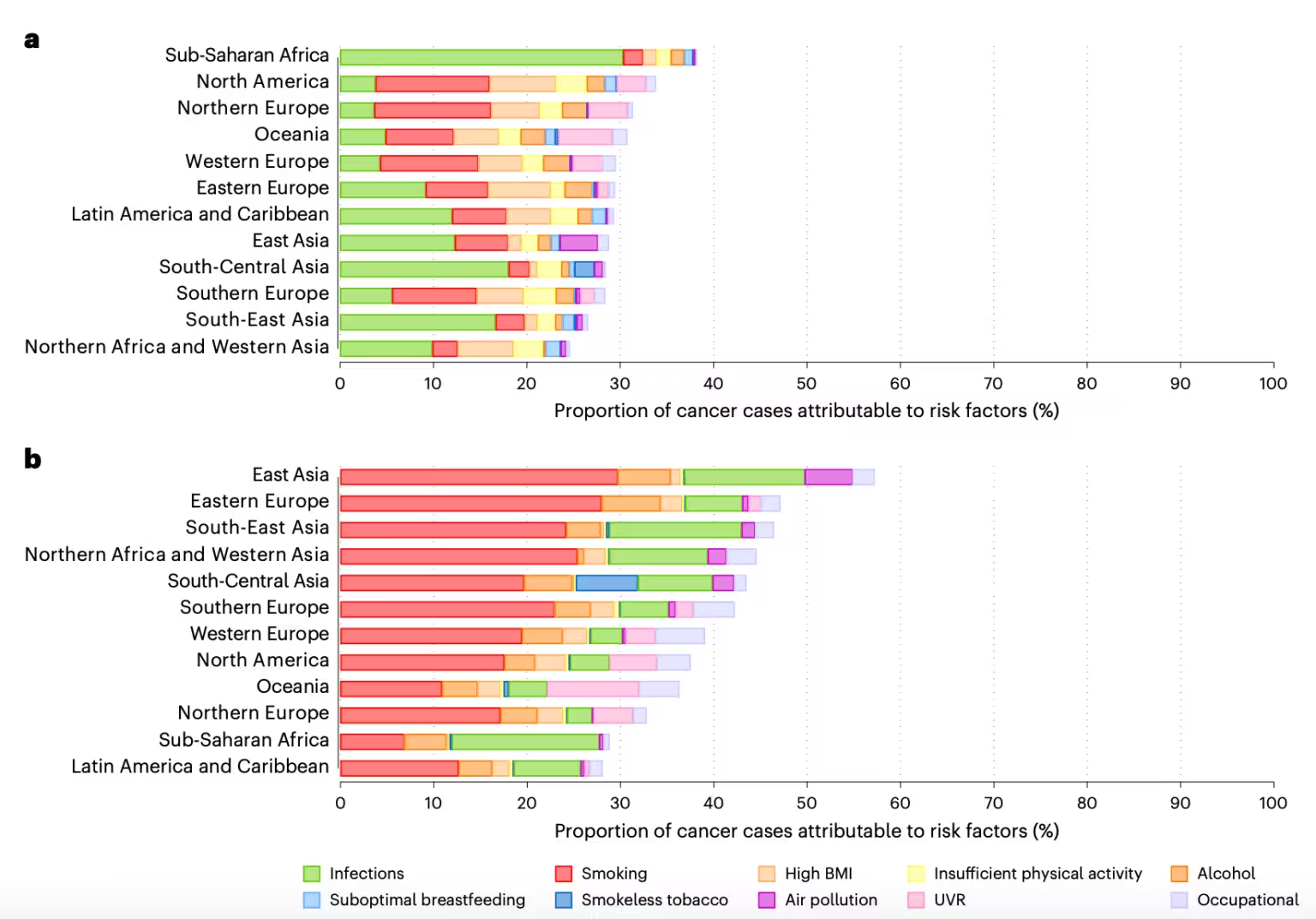
Infections also remain significant. Around 10 percent of new cancers were tied to infectious agents, with high-risk human papillomavirus (HPV) singled out as the dominant cause of preventable cancers among women because of its link to cervical cancer. An effective HPV vaccine exists and can prevent many of these cases, yet coverage gaps persist in many countries.
Other factors the analysis flagged include high body mass index, low physical activity, smokeless tobacco, the traditional stimulant areca nut, inadequate breastfeeding, ultraviolet radiation and more than a dozen occupational hazards. Stomach cancer, for instance, still shows higher incidence in men and is often associated with smoking and conditions tied to infection risks—crowding, poor sanitation and limited access to clean water.
Experts at WHO framed the finding as an opportunity. Isabelle Soerjomataram, a medical epidemiologist and senior author on the analysis, noted that addressing preventable causes is "one of the most powerful opportunities to reduce the global cancer burden." André Ilbawi, WHO's team lead for cancer control, emphasized that disaggregating risk patterns by country and population gives policymakers practical, targeted strategies to prevent cancers before they appear.
So what can societies do? Tobacco control remains the single highest-impact intervention: higher taxes, stronger advertising limits, smoking cessation services and plain packaging have all reduced tobacco use where they have been implemented. Expanding HPV vaccination and cervical screening, cutting harmful alcohol consumption, tightening air quality standards and improving sanitation in vulnerable communities are equally straightforward levers with proven effects. Occupational protections and monitoring can eliminate specific workplace carcinogens.
Numbers tell a simple story: prevention works, but only if politics, public health systems and communities act together. Reducing exposure to a handful of risk factors would prevent millions of cancers each year — and save countless lives. Will we treat that as an emergency or an option?
Source: sciencealert

Leave a Comment