5 Minutes
A recent case study has upended assumptions about a common group of human papillomaviruses (HPV). Researchers report that a beta-HPV — previously considered a weak cofactor that merely exacerbated UV damage — actually integrated into tumor DNA and promoted aggressive cutaneous squamous cell carcinoma (cSCC) in an immunodeficient patient. The finding highlights how hidden viral activity and immune defects can change both diagnosis and treatment strategies.
From a recurring forehead tumor to a surprising viral culprit
The story began with a 34-year-old woman whose forehead skin cancer kept returning despite repeated surgeries and immunotherapy. Her diagnosis: cutaneous squamous cell carcinoma (cSCC), one of the most common forms of skin cancer. Standard explanations like ultraviolet (UV) exposure and DNA-repair failure were considered. But genetic sequencing of the tumor revealed an unexpected player — beta-HPV sequences integrated into the tumor's genome and actively producing viral proteins.
Until now, integration of beta-HPV into human DNA had not been documented as a driver of sustained cancer growth. That distinction set this case apart from the well-established role of alpha-HPV types in cervical and oropharyngeal cancers, where viral integration and oncogene expression are known mechanisms.
Immune defect unlocked the virus
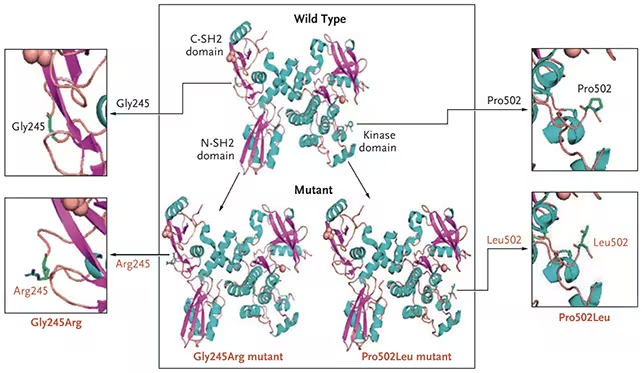
The patient carried an inherited immune disorder that impaired her T-cell response. Specifically, defects affecting the ZAP70 signaling protein were implicated — a molecular fault that prevented effective T-cell recognition and clearance of HPV-infected cells. Although her cells could still repair UV-induced DNA damage, the weakened adaptive immune surveillance allowed beta-HPV to invade skin cells and persist, ultimately tipping those cells toward malignant transformation.
“It suggests that there may be more people out there with aggressive forms of cSCC who have an underlying immune defect and could benefit from treatments targeting the immune system,” says immunologist Andrea Lisco from the U.S. National Institute of Allergy and Infectious Diseases (NIAID).
Treatment pivot: stem cell transplant and remission
Once the team identified the viral integration and the underlying T-cell dysfunction, clinicians moved beyond standard skin-cancer therapy. The patient received a bone marrow stem cell transplant to replace her defective immune cells with healthy donor-derived T cells. Following transplant, both the recurrent cSCC and the other HPV-related lesions — including skin and oral warts — resolved and did not recur during three years of follow-up.
“This discovery and successful outcome would not have been possible without the combined expertise of virologists, immunologists, oncologists, and transplant specialists, all working under the same roof,” Lisco added.
Why this changes how we think about some skin cancers
This case does not reduce the central role of UV radiation in skin cancer. Instead, it adds nuance: in certain immunocompromised individuals, normally low-risk viruses can become oncogenic drivers when immune surveillance fails. The implication is twofold. First, clinicians should consider viral testing and immune-genetic screening for patients with unusually aggressive or recurrent cSCC. Second, targeted immune-restorative treatments — including stem cell transplant or immune therapies tailored to the patient’s specific defect — may be more effective than repeated local treatments alone.
The report, published in The New England Journal of Medicine (Ye et al., 2025), also echoes a broader public-health success story: alpha-HPV vaccinations have led to dramatic declines in cervical and throat cancers. While vaccines for beta-HPV are not established, this case reinforces the potential value of virus-focused prevention and precision medicine.
Clinical and research implications
- Diagnostic protocols: Add viral genomic analysis when cSCC exhibits atypical behavior or treatment resistance.
- Genetic screening: Test for T-cell signaling defects (e.g., ZAP70-related pathways) in recurrent cases.
- Therapeutic strategies: Consider immune-reconstitution approaches — including hematopoietic stem cell transplant — for selected patients with confirmed viral-driven tumors.
- Surveillance and prevention: Research is needed to assess how common beta-HPV integration is across immunocompromised populations and whether targeted vaccines or antivirals could reduce risk.
Expert Insight
Dr. Maria Chen, a clinical immunologist and translational researcher not involved in the study, comments: “This report is a powerful reminder that cancer is often a disease of failed control systems — here, the immune system. When those control systems falter, microbes that are normally harmless can gain a foothold and drive malignant change. From a clinical standpoint, sequencing and immunophenotyping should become routine for atypical or refractory skin cancers.”
The case is a call to integrate virology, immunology, and oncology more tightly. For patients whose cancers refuse to behave, looking beyond the tumor itself — at the genome, the viruses living in tissues, and the patient’s immune wiring — can reveal treatable causes and durable cures.
Source: sciencealert
Comments
Reza
is this common or a freak case? if that s true, should we screen every recurrent cSCC patient for viruses and immune genes… transplants tho, huge risk.
bioNix
Wow, never thought a beta HPV could actually integrate and drive skin cancer. The stem cell fix sounds unreal, kinda gives hope but also scary... weird how hidden infections + immune gaps change the whole game!

Leave a Comment