5 Minutes
Chemotherapy can leave patients with lasting nerve pain that looks a lot like a direct injury to nerves — but new research suggests the real culprit may be an immune system stress response. Scientists have identified a molecular “alarm” inside immune cells that, when triggered by certain chemotherapy drugs, sets off inflammation and harms sensory nerves. Blocking that alarm could protect patients and help them complete life-saving cancer treatment.
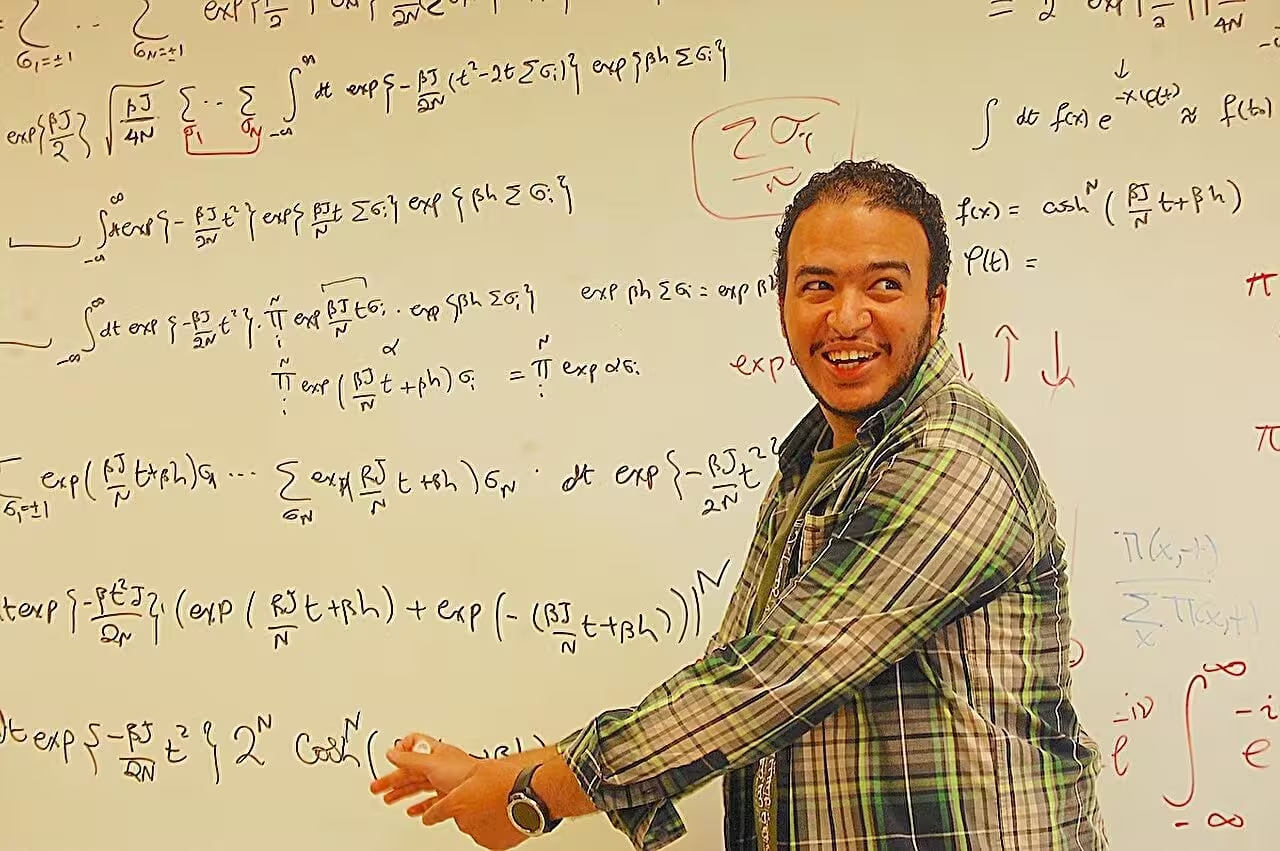
Chemotherapy may cause nerve pain by triggering a stress response in immune cells rather than directly damaging nerves. Shutting down this response could help protect patients from one of treatment’s most debilitating side effects. Credit: Shutterstock
How chemo flips the immune alarm and leads to pain
Up to half of people who receive chemotherapy develop chemotherapy-induced peripheral neuropathy (CIPN), a condition characterized by tingling, numbness and burning pain in the hands and feet. Until now, the mechanism behind many cases of CIPN has been unclear, and effective therapies are limited. Researchers at Weill Cornell Medicine and Wake Forest University have traced a biological chain reaction that begins not in neurons but inside immune cells.
What is the IRE1α-XBP1 pathway?
The team focused on a cellular stress pathway called IRE1α-XBP1, an internal sensor that tells cells they are under duress. When immune cells experience oxidative stress — for example, from reactive oxygen species generated after exposure to the chemotherapy drug paclitaxel — IRE1α activates and drives a gene program mediated by XBP1. That response pushes immune cells into a hyperinflammatory state.
Rather than attacking cancer directly, these overactive immune cells migrate to the dorsal root ganglia — sensory nerve clusters that relay information from the limbs to the spinal cord — and release inflammatory factors that damage nearby nerve fibers. The result is the typical CIPN picture: pain, cold sensitivity and loss of nerve endings.
Blocking the stress signal: experiments that reshaped the story
In mouse models that mimic patient symptoms, the researchers tested both genetic and pharmacologic ways to silence IRE1α in immune cells. Turning off the pathway genetically prevented the inflammatory cascade and preserved nerve health. Importantly, a small-molecule IRE1α inhibitor — already being evaluated in early clinical trials for some solid tumors — produced similar protective effects when given alongside paclitaxel.
Mice that received the IRE1α inhibitor showed fewer pain behaviors, maintained more nerve fibers, and had reduced immune-driven inflammation in the dorsal root ganglia. Those results suggest a practical strategy: repurpose or co-administer IRE1α-targeting drugs to reduce neuropathy in patients treated with taxane chemotherapies.
“We found a mechanism that maps specifically to immune cells, not neurons,” explained Dr. Juan Cubillos-Ruiz of Weill Cornell Medicine, summarizing the shift in thinking. Co-leader Dr. E. Alfonso Romero-Sandoval of Wake Forest added that targeting immune stress responses could change how clinicians prevent and manage CIPN.
Early patient signals and the prospect of a predictive blood test
To bridge lab and clinic, the team ran a pilot study in women receiving paclitaxel for gynecologic cancers. Blood taken before and during chemotherapy cycles showed that patients who later developed severe neuropathy already had higher activity of the IRE1α-XBP1 pathway in circulating immune cells. This raises the possibility of a predictive biomarker: a blood assay that flags high-risk patients before nerve damage becomes clinically apparent.
If validated in larger studies, such a test could enable clinicians to tailor treatment plans — from closer monitoring and dose adjustments to preemptive use of IRE1α inhibitors — protecting quality of life without compromising anticancer efficacy.
Related technologies and clinical implications
The translational appeal is twofold. First, some IRE1α inhibitors are already in phase 1 trials for cancer, which could accelerate repurposing studies focused on neuropathy prevention. Second, a validated biomarker would support precision medicine: identifying patients who most need neuroprotective strategies and reserving experimental approaches for those at lowest risk.
Beyond taxanes, the insight that immune stress responses — not only direct nerve toxicity — contribute to CIPN may prompt reexamination of other chemotherapy agents and supportive drugs. Combining anti-stress agents with established symptomatic therapies could produce better outcomes than current standards of care.
Expert Insight
"This work reframes peripheral neuropathy from a neuron-centered problem to one that involves the immune system's stress machinery," says Dr. Lisa Carver, a clinical neuroimmunologist (expert commentary). "If further clinical trials confirm safety and efficacy, targeting IRE1α could become a preventive strategy that preserves patients' mobility and ability to complete chemotherapy. That would be a major win for survivorship care."
Looking ahead, researchers stress the need for larger patient cohorts and carefully designed trials to test whether IRE1α inhibitors can be safely combined with different chemotherapy regimens. If successful, the approach could reduce treatment interruptions, improve adherence to curative regimens, and decrease long-term disability from chemo-related nerve injury.
Source: scitechdaily
Comments
Armin
Is this even proven in humans? Pilot was tiny. Curious about long term effects of blocking IRE1alpha though, no surprises pls.
labcore
Wow, didnt expect chemo pain to be immune driven... that could change everything, fingers crossed but cautious.


Leave a Comment